
views
X
Research source
In most cases, only the skin is frozen (known as frostnip) but in extreme cases dead tissue goes deeper and must be handled delicately. Frostbite requires careful medical attention to minimize damage and reduce the likelihood of further harm.
Determining the Severity

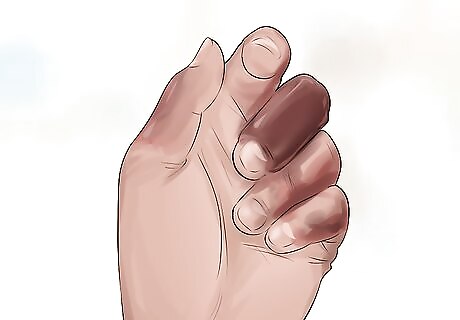
Determine if you have frostnip. Frostnip is not the same as frostbite, but can precede it. Ice crystals form on the surface of the skin, rather than within the tissue as in frostbite. The blood vessels in your skin severely constrict, causing paleness or reddened areas. You may feel numbness, pain, or prickling or tingling of the area. However, the skin should respond normally to pressure without serious numbness and should retain its normal texture. Symptoms resolve with rewarming. Frostnip may affect children more quickly than adults. Frostnip usually affects extremities such as the ears, nose, fingers, toes, and cheeks. Frostnip signals that weather conditions are sufficient to cause frostbite with further exposure.

Determine if you have superficial frostbite. Although it may not feel superficial, superficial frostbite is so named because the damage can be reversed with treatment. This condition is more serious than frostnip, and can be recognized by numbness, white or grayish-yellow skin with red blotches, aching or throbbing, and slightly hardened or swollen skin. There is less possibility of tissue loss with superficial frostbite. Some people with superficial frostbite may develop blisters with clear fluid within 24 hours. These are usually located at the ends or tips of the area affected and do not lead to tissue loss.
Determine if you have severe frostbite. Severe frostbite is the most dangerous form of frostbite. In cases of severe frostbite the skin looks pale and will feel waxy and unusually firm, and there is a loss of feeling/numbness of the affected area. In some cases, severely frostbitten tissue may have blisters on the skin that may have blood in them, or signs of gangrene (gray/black dead skin). The most severe form of frostbite extends into the muscle and bone and can lead to death of the skin and tissues. The risk of tissue loss is high with this form.

Get out of the cold and seek treatment as soon as possible. If you are able to get to a hospital or emergency department within two hours, you should not try to treat frostbite yourself. If you are unable to get out of the cold, do not try rewarming the area if it is in danger of refreezing. The freeze-thaw-freeze-thaw cycle causes more damage to your tissue than allowing it to simply remain frozen. If you are more than two hours away from medical treatment, you can begin treatment yourself. All three conditions -- frostnip, superficial frostbite, and severe frostbite -- have the same basic procedure for “field treatment” (away from a hospital).
Rewarming the Area
Begin warming up the affected area. As soon as you notice the frostbitten areas on your body (most commonly on the fingers, toes, ears, and nose), you should take steps to warm them up. Tuck fingers/hands into your armpits, and hold dry gloved hands over your face, toes, or other areas of the body to add heat. If you have any on, remove your wet clothes as these will prevent your temperature from rising.
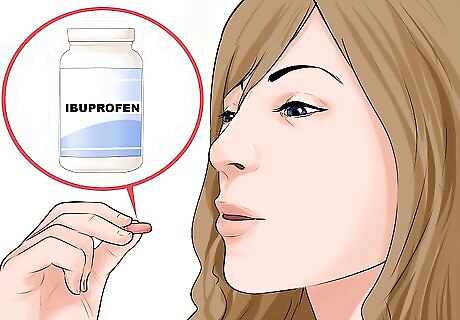
Take pain medication if necessary. If you’re suffering superficial to severe frostbite, the rewarming process may be painful. To prevent further suffering on your part, take an NSAID (nonsteroidal anti-inflammatory drug) pain reliever such as ibuprofen. However, do not take aspirin, as it may keep your body from healing effectively. Follow the bottle instructions for dosage amounts.

Rewarm the frostbitten area by submerging it in warm water. Fill a basin or bowl with water at a temperature between 104-107.6 degrees Fahrenheit (40-42 degrees Celsius). Water at a temperature of 104.9 (40.5 degrees Celsius) is considered ideal. Do not use temperatures above these, as this could burn the skin and cause blisters. If it is available, add antibacterial soap to the water to help prevent infection. Submerge the affected area for 15-30 minutes. If you do not have a thermometer handy, test the water by placing an uninjured area such as a hand or elbow in the water. It should feel very warm, but still tolerable. If the water is painfully hot, cool the water a little bit. If possible, use circulating water rather than still. A whirlpool bath is ideal, but even using running water would work. Do not allow the frozen area to touch the sides of the bowl or vessel. This could cause damage to the skin. Do not rewarm the area for less than 15-30 minutes. As the area thaws, you may experience severe pain. However, it is important to continue rewarming the area until it is fully thawed. If you stop the rewarming process too early you could cause further damage. For severe frostbite, you may need to rewarm the area for up to an hour.

Do not use dry heat such as heaters, fireplaces or heating pads. These heat sources are too difficult to control and will not supply the sort of gradual heat needed to treat frostbite. They can also cause burns. Remember that the frostbitten area will be numb, and you will be unable to gauge the temperature. Dry heat sources cannot be accurately monitored.

Pay attention to the frostbitten areas. As your skin begins to rewarm itself, you should feel tingling and burning sensations. The frostbitten area should turn pink or red, often blotchy, and regain a regular texture/feeling. Your skin should not swell or blister; these are signals of further damage that should be treated immediately by a doctor. Additionally, if your skin does not change at all after several minutes in warm water, there may be significant damage that your doctor needs to treat. Take photos of the affected area if possible. This will help your doctor track the progress of the frostbite and determine whether it is improving with treatment.

Prevent further damage. Continue to seek medical attention, but in the process keep from worsening your frostbite. Don’t rub or chafe the frostbitten skin, avoid too much movement, and don’t allow the area to be affected by extreme cold again. Allow the rewarmed areas to air-dry or gently blot them dry with a clean towel, but do not rub them. Do not bandage the area yourself. There is no evidence that supports bandaging a frostbitten area before getting proper medical treatment, and bandaging may interfere with your mobility. Do not massage the frostbitten area. This can cause further tissue damage. Elevate the area to help reduce swelling.
Getting Professional Treatment

Get further medical treatment. Depending on the severity of your frostbite, the treatment you receive from your doctor may vary. Hydrotherapy is most common, but in extreme cases surgery is provided. If you suffered from severe frostbite, your doctor may be limited to amputation as a treatment option, but this decision is only made 1-3 months after the initial exposure, once the full extent of tissue damage is clear. Your doctor will ensure that proper rewarming has taken place and assess any “non-viable tissue,” or tissue that was unable to be healed. When your treatments are done and you are ready to be released from the hospital or emergency department, the doctor will bandage the damaged area and provide specific instructions for what precautions you should take as you recover. This will vary, depending on the severity of your frostbite. If you have severe frostbite, your doctor may recommend transferring you to a burn unit for treatment. You will need to follow up with your doctor within 1-2 days after leaving the hospital or emergency department if you have moderate or severe frostbite. Extremely severe conditions will require more follow-up at 10 days and 2-3 weeks.

Talk to your doctor about aftercare. Because your skin was damaged by the frostbite, it is at risk of further damage as you begin to heal. You will probably also experience some pain and inflammation as you heal. Get plenty of rest, and talk to your doctor about the following: Applying aloe vera. Studies suggest that applying pure aloe vera cream to the affected areas may help prevent further skin damage and increase tissue healing. Managing blisters. Your skin will likely blister as you recover. Do not pop or break blisters that appear. Ask your doctor how to handle them until they break on their own. Managing pain. Your doctor will likely prescribe ibuprofen to help manage pain and inflammation. Take it as directed. Preventing infection. Especially in severe cases, your doctor may prescribe antibiotics. It is important to take the full course of antibiotics exactly as prescribed. Getting around. If your frostbite affected your feet or toes, you should avoid walking on them as you heal. Walking on frostbitten areas can cause further damage. Ask your doctor about a wheelchair or other options.
Protect the area from further cold. To assure your full recovery and prevent further damage, you need to protect the affected area from further cold exposure for 6-12 months. To prevent future incidents of frostbite, limit your time outdoors in very cold weather, especially if it is windy or wet.













Comments
0 comment