views
- Stay hydrated, try a saline nasal rinse, or sit in a steamy shower to relieve postnasal drip.
- Some decongestants can make your postnasal drip worse if you overuse them.
- Keep your home environment free of irritants and allergens to prevent postnasal drip.
- The best treatment for chronic postnasal drip depends on what’s causing your symptoms, so consult your doctor.
Using At-Home, Doctor-Recommended Treatments
Drink plenty of fluids to remain hydrated. Dehydration can aggravate the symptoms of rhinitis and postnasal drip. Avoid caffeine and alcohol, which can cause dehydration. Water is the best choice to remain hydrated while suffering from rhinitis and postnasal drip. Look at your urine to determine if you're getting enough water during the day. If your urine is yellow, you're probably not getting enough water. If your urine is clearer, with at most a hint of yellow, you're probably drinking enough water. Drinking warm fluids, such as warm water, hot decaf tea, or clear broth, is especially helpful for relieving postnasal drip.

Make a saltwater gargle. Add 1/2 teaspoon (3g) of salt to 8 fluid ounces (240 mL) of warm or lukewarm water and gargle after lifting your head back. Do this 3 to 4 times a day.

Use steam treatments. Try out a DIY steam treatment by covering your head with a towel and placing it a safe distance from a pot of warm water. Take a warm shower. Let the steam of the warm water work its way into your lungs and sinuses while you bathe.
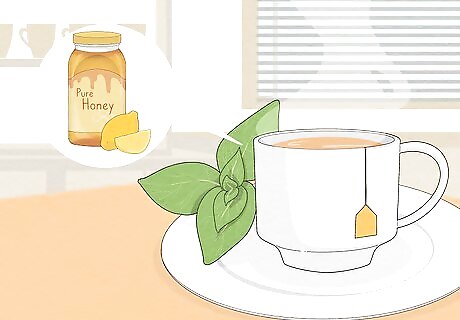
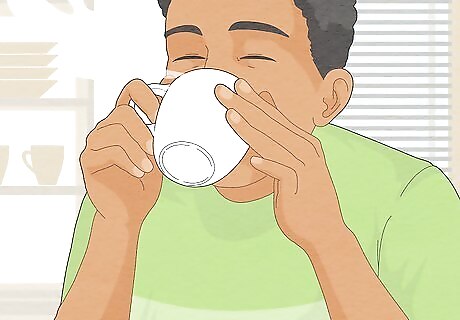
Drink hot tea with honey and lemon. This traditional cold remedy is great for breaking up mucus, and it will also help soothe the sore throat that often comes with postnasal drip. Choose an herbal or decaffeinated tea, since caffeine can make your congestion worse. Some people swear by lime juice as a remedy for congestion. While there’s not a lot of evidence to support the “lime cure,” it’s possible that the immune-boosting properties of citrus might help with colds and other causes of the sniffles. Try mixing a little lime juice into your tea.
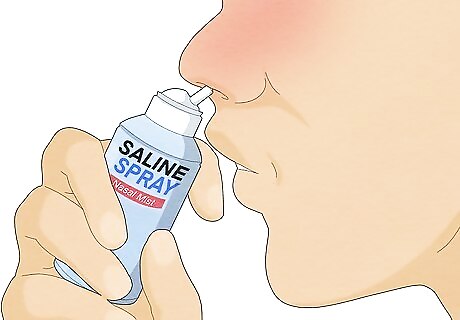
Rinse the nasal cavity to remove mucus-causing irritants. Over-the-counter saline kits like the ones here and nasal sprays like the ones here are available to rinse the nasal cavity. The saline solution flushes the irritants from the nasal cavity, thins the mucus, and relieves the membranes in the nose. Try using a Neti pot to clear out the mucus in the sinus and the back of the throat. You can find a variety of Neti pots on Amazon here. Be aware, however, that by using a sinus irrigation device you could be removing natural antimicrobial agents that get rid of enemy bacteria, viruses, and fungi. Apply 2 to 3 saline nasal drops every 2 to 3 hours to help moisten your nasal passages and relieve congestion.
Avoid caffeine, alcohol, and spicy foods. All 3 may make mucus production worse, so it is best to avoid these while you have a cold.

Blow your nose frequently to remove excess mucus in the nasal cavity. Blowing your nose can remove irritants, which cause a buildup of mucus. For mucus that cannot be cleared after blowing the nose, some people prefer snorting and spitting the excess mucus from the back of the throat, avoiding bad breath and dry mouth.

Use over-the-counter decongestants with caution to relieve mucus buildup and postnasal drip. Oral decongestants narrow the blood vessels to reduce the amount of congestion in the nasal cavity. Decongestants are also available in a nasal spray. Use decongestant sprays for no more than 3 days in a row. If symptoms don't get better after 3 days, discontinue the use of medicated decongestant sprays or drops. Using these kinds of decongestants for longer than 3 days can cause “rebound congestion,” which may persist for months. Rebound congestion happens when your body grows dependent on decongestant sprays or drops, causing you to feel even stuffier when you stop taking them.

Remove mucus with mucus-thinning medications. Medications such as guaifenesin (Mucinex) are sold over-the-counter and taken in tablet or syrup form. These help to thin out the mucus and make it easier for it to run out. Follow the manufacturer’s instructions for how to take these medications and ask your doctor or pharmacist if you are unsure.
Do a round of house cleaning. If allergens are haunting your sinuses, the only home treatment you may need is a deep clean of your home. Try the following suggestions to remove dust, pollen, and dander from your residence before they come back to bite you—in the nose. Wash your clothes, sheets, pillowcases, and mattresses in hot water regularly. Hot water will kill any bacteria that may be causing your symptoms. Vacuum regularly with true or absolute HEPA filters. Vacuuming with HEPA filters ensures that any allergens are picked up during the vacuuming process.
Ask your doctor about herbal remedies. Some herbs, like sorrel and cowslip, may help loosen mucus and minimize the symptoms of post-nasal drip. However, always talk to your doctor before trying any new herbal remedy. Let them know if you’re taking any other medications, since some herbs can interact with over-the-counter or prescription drugs. If your doctor says it’s okay, try herbal blends like Sinupret that are designed to clear your sinuses and help mucus drain more effectively.
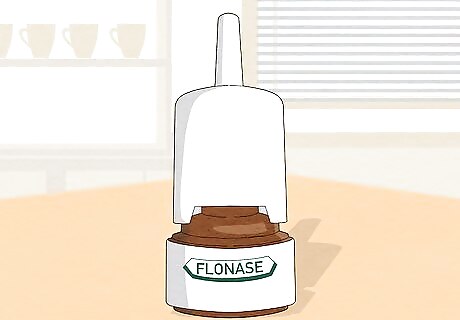
Ask your doctor for prescription medications to relieve recurring irritation and mucus buildup. Your physician can prescribe corticosteroid, antihistamine, and anti-drip sprays to relieve postnasal drip. Corticosteroid sprays, such as Flonase and Nasacort, help to treat the swelling and inflammation in your nasal passages that occur with allergic rhinitis. Antihistamine sprays can effectively treat allergic rhinitis and are also effective for some non-allergic causes of postnasal drip, such as vasomotor rhinitis, which must be evaluated by your allergist.
Preventing Postnasal Drip

Remove allergens from the environment when possible. Allergens such as dust, pollen, pet dander, and mold can irritate the nasal cavity and lead to postnasal drip. If you have allergies, the best way to prevent postnasal drip is to keep your environment free of irritants and allergens. Bathe your pets often because dander from their saliva and skin glands may cause irritation leading to postnasal drip. It may be necessary to remove pets from the home if the allergic reaction and postnasal drip are severe. Remove flowering and non-flowering plants from the home. Enclose unused pillows and mattresses in plastic to minimize allergens while sleeping. Vacuum compression bags like these on Amazon are a good option for storage. Clean your living areas by sweeping, mopping, and dusting. Launder and change your bedding frequently.

Use a HEPA air purifier. These filters help remove allergenic irritants from the environment. Luckily, there are not big differences between the very expensive and budget ones. Keep an air purifier in your bedroom and any other parts of your home where you spend a lot of time during the day. Make sure to keep it on while you sleep as well. Some top-rated options on Amazon include the Levoit purifier and Aroeve purifier for cheaper options, or the Veva purifier for quiet operation, and the Bissell purifier for ease of use. In addition, using a humidifier can add moisture to the air, which relieves the irritation in the nasal cavity. When the nasal cavity is irritated, it produces excess mucus as a response. If you don’t have a humidifier, take a hot shower and inhale the steam.
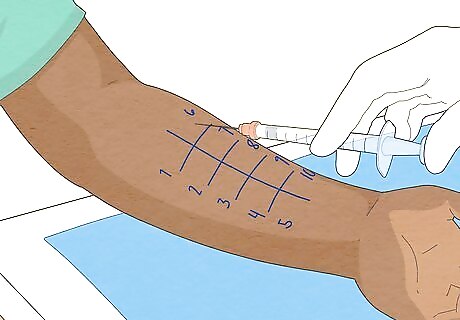
Consult an allergist or take an allergy test. Chronic postnasal drip could be caused by an underlying food allergy that you don't yet know about or have recently developed. Check with an allergist to see if you could be allergic to something and not yet know it. If you have postnasal drip with temperature changes, let the allergist know as you might have a non-allergic condition called vasomotor rhinitis. Dairy is not a likely culprit, and studies indicate no clear link between dairy and mucus production.

















Comments
0 comment