
views
X
Trustworthy Source
Harvard Medical School
Harvard Medical School's Educational Site for the Public
Go to source
Getting a proper diagnosis of your calf muscle strain is crucial because it determines the type of treatment protocols you should follow.
Consulting With Professionals

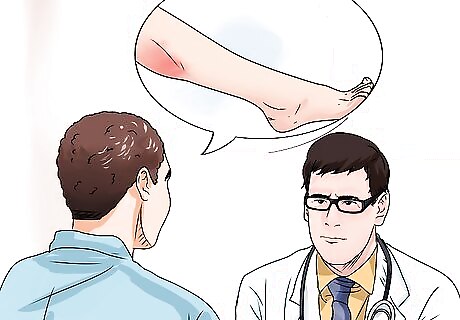
Schedule an appointment with your doctor. If you develop calf pain that won't go away after a few days, then schedule an appointment with your family physician. Your doctor will examine your leg and calf muscles, ask questions about your lifestyle and how you might have injured it, and maybe even take X-rays of your lower leg (to rule out a fracture of the tibia and fibula bones). If necessary, your doctor will refer you to a musculoskeletal specialist, who has more specialized training. Other types of healthcare professionals who could help diagnose and treat musculoskeletal injuries include osteopaths, chiropractors, physiotherapists and massage therapists. However, you should always start with your doctor, as he can also rule out other, potentially serious causes of pain, such as blood clots, vascular injury, baker's cysts, or a potential surgical emergency like compartment syndrome.

See a specialist about your leg. Calf muscle injuries are usually just mild Grade I strains, but sometimes surgery is required if the muscles are badly torn. Furthermore, some serious medical conditions can cause calf pain or refer pain to that region, such as a bone fracture, bone cancer, bone infection (osteomyelitis), venous insufficiency, sciatica from a lumbar disc herniation or complications related to diabetes. As such, medical specialists such as an orthopedist (bone and joint specialist), neurologist (nerve specialist) or physiatrist (muscle and bone specialist) may be needed to rule out the most serious causes of your calf pain. X-rays, bone scans, MRI, CT scan and ultrasound are modalities that specialists may use to help diagnose your lower leg pain. Calf muscle injuries are relatively common among those who play tennis, basketball, football, soccer and volleyball, as well as those who run track and field.
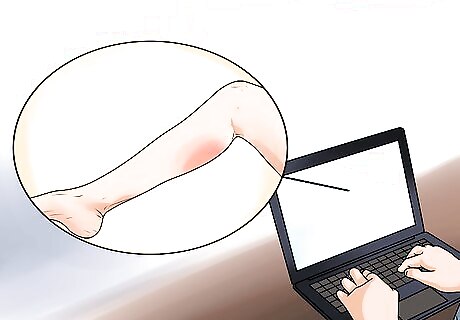
Understand the various types of treatments available. Make sure you get the doctor to clearly explain the diagnosis, especially the cause (if possible), and provide you with various treatment options for your condition. Rest and home care modalities (such as ice) are appropriate for mild-to-moderate calf muscle strains. Research calf injuries on the internet (only medically reputable sites) in order to flesh out your understanding of the condition and learn more about treatments and their expected outcomes. Factors that can predispose someone to a muscle strain (or "pull") include older age, previous muscle injury, less flexibility, lack of strength in the muscle and fatigue.
Treating Grade I Calf Strains
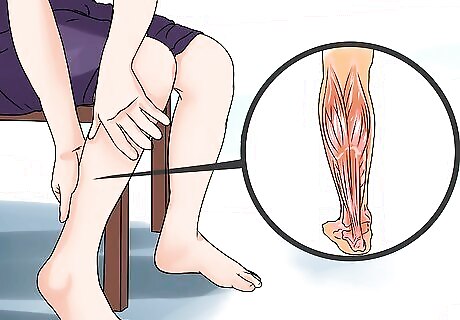
Identify the seriousness of the injury. Most calf strains are minor injuries and self-heal within a week -- the degree of pain, disability and bruising are good indicators of seriousness. Grade I muscle strains involve micro-tears of up to 10% of the muscle fibers. They're characterized by mild pain twinges at the back of the lower leg, usually in the mid to proximal (closer to the knee) region of the leg. Minimal loss of strength and motion is experienced. You may still be able to walk, run or play your sport, albeit with discomfort and tightness. Muscle strains occur when the force in the muscle is so great that the tissue tears, most commonly at the junction between where the muscles taper into tendons. Most Grade I lower leg strains cause discomfort for between two to five days post injury, but may take a few weeks to fully heal, depending on proportion of muscle fibers involved and the type of treatment sought. Injuries can even happen to seasoned athletes. "I have been victim to several calf strains/sprains over my nearly seventy years. The first serious one happened at age 15 when running the last bend in a 4 x 100m relay (we got Gold!), and the most recent happened last Saturday afternoon. I have always been very active in sports (rugby till injury stopped me playing at 54, and squash until 60, so in some ways the calf issues were almost inevitable). This article helped me identify and heal my strain." - David D. Identify your strain to create a path to recovery. "I learned that there are two primary calf muscles and three classifications for muscle strain. What really helped me is learning about a grade 2 calf strain. I was able to return to full activity when the pain went away." - Dan D. Did you know that wikiHow has collected over 365,000 reader stories since it started in 2005? We’d love to hear from you! Share your story here.

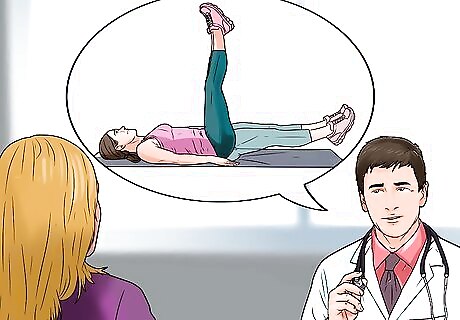
Utilize the R.I.C.E. treatment protocol. The most effective treatment protocol for most sprain / strain injuries is abbreviated R.I.C.E. and stands for rest, ice, compression and elevation. The first step is rest — temporarily stop all activity in order to address your injury. Next, cold therapy (ice wrapped in a thin towel or frozen gel packs) should be applied to the injury as soon as possible in order to stop any internal bleeding and reduce inflammation, preferably while your leg is elevated on a chair or stack of pillows (which also combats inflammation). Ice should be applied for 10 –15 minutes every hour, then reduce the frequency as the pain and swelling subside over the course of a few days. Compressing the ice against your injury with a compression bandage or elastic support will also help stop the bleeding from the torn muscle fibers and associated inflammation. Don't tie the compression bandage too tight or leave it on for more than 15 minutes at a time because complete restriction of blood flow could cause more damage to your leg.
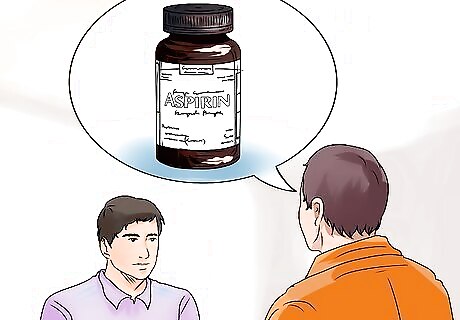
Take over-the-counter medications. Your family doctor may recommend anti-inflammatories such as ibuprofen, naproxen or aspirin, or possibly regular analgesics (pain killers) such as acetaminophen to help combat the inflammation and pain associated with your calf injury. Keep in mind these medications are hard on your stomach, liver and kidneys, so they should be taken for no more than two weeks at a time unless otherwise directed by your doctor.

Practice calf stretches. Mild muscle strains respond well to some light stretching because it relieves muscle tension and promotes blood flow. Following the inflammatory phase of a muscle strain injury, some scar tissue forms, which is not as flexible as muscle fiber. Stretching helps the scar tissue remodel and become more flexible. Thus, take a towel or compression bandage and wrap it underneath your foot nearer the toes. Then grab each end with your hands and slowly pull back while slowly extending your leg and noting the deep stretch in your calf muscles — hold for 20-30 seconds and then slowly release. Practice this stretch three to five times daily for one week, as long as your calf pain isn't exacerbated by it.
Consult your doctor or a physical therapist prior to doing this and use great caution, as performing these exercises can sometimes worsen the situation and prolong your healing and recovery. Warming up then stretching your calf muscles prior to any athletic activity may help prevent injuries such as strains, sprains and muscle cramps.
Treating Grade II Calf Strains
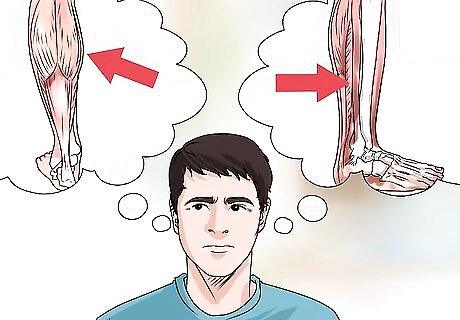
Differentiate between gastrocnemius vs. soleus strain. With a more serious strain, it's important to distinguish which muscle is involved to the greater extent: the deeper soleus or the more superficial "heads" of the gastrocnemius. MRI or diagnostic ultrasound may be needed to best diagnose the location and degree of the injury. Grade II strains involve more extensive damage, up to 90% of the muscle fibers may be torn. These injuries present with more pain (described as sharp in nature), significant loss of muscle strength and range of motion. Swelling is more severe and bruising quickly develops because of the internal bleeding from the torn muscle fibers. With Grade II strains, there's limited ability to perform activities, especially jumping and running, so you'll be sidelined for a while (a few weeks or more). The gastrocnemius muscle is considered at high risk for strains because it crosses two joints (knee and ankle) and has a high proportion of type-2 fast twitch muscle fibers. The medial head of the gastrocnemius muscle is strained more often than the lateral head.
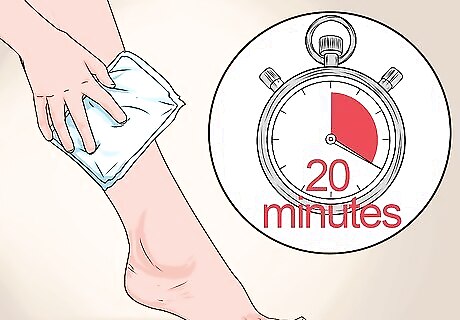
Utilize the R.I.C.E. treatment protocol. This protocol is still appropriate for Grade II strains, although you may have to keep the ice on your calf for a little longer (up to 20 minutes at a time) if the deeper soleus muscle is the primary site of injury. Instead of using R.I.C.E for a few days as is the case with a mild strain, more severe strains will likely require attention for a week or more. Most Grade II lower leg strains cause significant discomfort for between one to two weeks post injury, depending on proportion of muscle fibers involved and the type of treatment sought. These types of muscle injuries may require one to two months before a complete return to athletics occurs. For moderate to severe muscle strains, the use of anti-inflammatories should be restricted in the first 24 – 72 hours due to increased risk of bleeding from the anti-platelet (blood thinning) effect.
Seek out physical therapy. A Grade II strain is a relatively serious musculoskeletal injury that most likely involves significant scar tissue formation, as well as noticeably reduced range of motion and strength. As such, after the swelling, bruising and pain have mostly subsided, ask your doctor for a referral to a sports medicine specialist or physiotherapist who can offer a variety of tailored strengthening exercises, stretches, massage techniques and therapies such as therapeutic ultrasound (to reduce inflammation and break down scar tissue adhesions) and electronic muscle stimulation (to strengthen muscle fibers and promote blood flow). Return to full activity is usually allowed when you're pain free, have full range of motion of your lower leg and full strength of your calf muscles, which may take a few weeks or more. Calf strains are most common in men between the ages of 30 and 50 years.
Treating Grade III Calf Strains

Seek medical attention immediately. A Grade III strain is a complete rupture of the muscle body or tendon. It involves significant pain (burning and/or sharp in nature), immediately severe inflammation and bruising, muscle spasms and sometimes an audible "pop" as the muscle is severed. There is also a palpable bulging defect in the calf as the larger severed portion strongly contracts. An inability to walk is characteristic of a Grade III calf strain, so assistance is usually needed to get to a hospital or clinic. The muscle fibers cannot reattach on their own, even with the help of scar tissue, so emergency intervention is required. A sudden tendon rupture (such as the Achilles tendon) is often excruciating and feels like someone has shot you from behind or struck you with something sharp. A severely strained calf will likely cause bruising, which will settle into your foot and turn it black and blue.
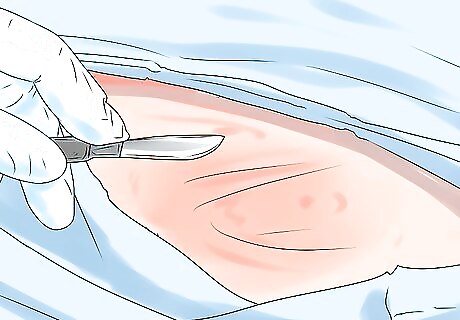
Get surgical repairs. Grade III (and some Grade II) strains may require surgery to repair and reattach the damaged calf muscle and/or tendon. Time is of the essence because the longer a muscle is ruptured and severely contracted, the more difficult it is to stretch out and achieve normal muscle tone. Furthermore, internal bleeding can cause local necrosis (surrounding tissue death) and possibly (though very rarely) even lead to anemia from blood loss. Ruptures within the belly of a muscle heal quicker because of the better blood supply, whereas tendon ruptures don't receive as much blood and take longer to heal. Revert to the R.I.C.E. protocol following surgery. In the case of complete ruptures, the calf muscles take about 3 months or so to heal following surgery and rehabilitation. Post surgery, you'll likely wear a supportive compression boot and have to use crutches over the short term before progressing to physical therapy exercises.
Spend time rehabilitating. Much like a Grade II strain, physical therapy is needed to heal a Grade III sprain, especially if surgery is needed. Under the guidance of a physiotherapist or physiatrist, tailored isometric, isotonic, and then dynamic training exercises can be added in a consecutive manner as each type of exercise is completed without pain. These exercises will strengthen the calf muscles and return them to form. Return to athletic activity can resume slowly within 3-4 months, although there will always be a greater risk of re-injury in the future. Poor biomechanics or foot posture contribute to calf injuries, so you may be fit with custom foot orthotics after your rehabilitation to prevent further problems.














Comments
0 comment