
views
Recognizing the Symptoms of Blood Clots
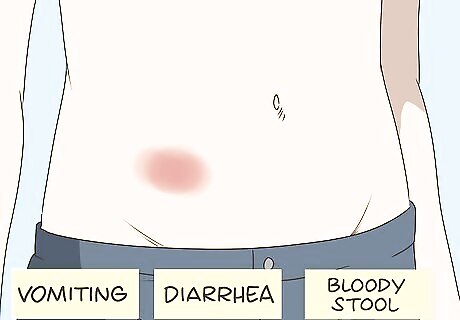
Know that clots in the abdominal area can produce severe pain and gastrointestinal problems. The symptoms of a blood clot vary depending on the clot’s location in the body. If the artery affected is responsible for supplying blood in the bowel, symptoms typically include sharp, excruciating abdominal pain. In addition, you may notice the following symptoms: Vomiting. Abdominal blood clots irritate the stomach lining, and the body responds by vomiting. Diarrhea. Lack of blood supply alters the function of the digestive system and often leads to diarrhea. Bloody stool. Any irritation to the linings of the digestive system can cause bleeding. You may therefore notice blood in your bowel movements.
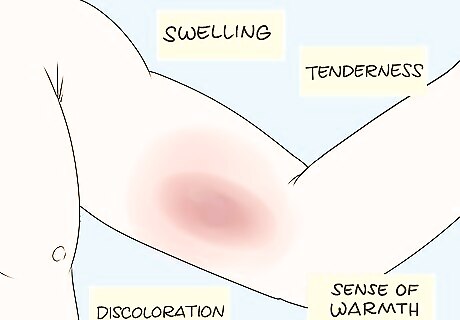
Understand that clots in the limbs can produce pain, swelling, and other distinctive symptoms. Blood clot formation in the arms or legs can block the blood flow returning to the heart. It will cause inflammation of the vein as well. You may notice a sudden, sharp pain, caused by deprivation of oxygen due to loss of blood supply. In addition, you may have the following symptoms: Swelling. When a vein is blocked, it will cause fluid retention and swelling in the area of the clot. Tenderness. In addition (or instead of) sharp pain, you may have a general discomfort or tenderness in the area. This happens because of the inflammation in the area. Discoloration. The clot blocks blood supply to the area, so the skin of your arm or leg may become bluish or red. A sense of warmth. When inflammation occurs, the body increases blood flow to the damaged area. The blood carries body heat from the core of the body, causing a warm sensation in the affected area.
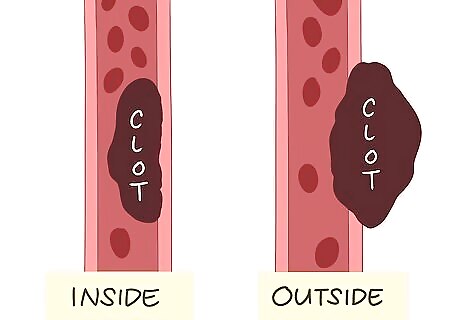
Understand that clots can be inside or outside a vein or artery. When a clot is inside a blood vessel it may partially or completely block blood flow, or become dislodged and lead to complications like stroke, pulmonary embolism or a heart attack. When the clot is outside the blood vessel it can still partially or completely block blood flow by putting pressure on nearby vessels.
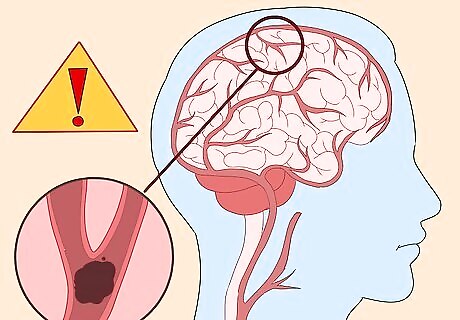
Be aware that clots in the brain can lead to a variety of frightening symptoms. The brain controls the body’s functions. If a clot impedes the flow of blood to the brain, it can affect sight, speech, and virtually all other functions of the body. This can result in a stroke. As a result, you may experience: Visual disturbances. Weakness. Paralysis. Seizures. Speech impairment. Disorientation.

Recognize that chest pain, shortness of breath, and sweating may signify a blood clot in the heart. When clots develop in the heart, it can cause an irregular rhythm and block the flow of blood. This leads to chest pain (which may radiate to the arms, back, neck or jaw), shortness of breath, and sweating. Clots in the heart can lead to life-threatening problems, such as a heart attack.
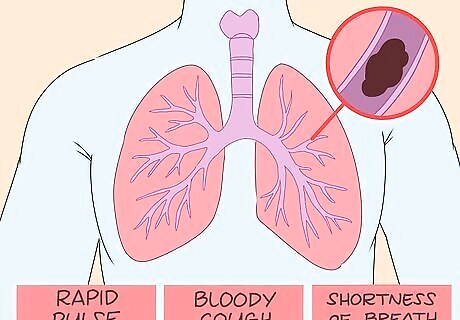
Know that blood clots in the lungs can cause chest pain and a variety of other symptoms. As with clots in the heart, clots in the lungs may cause severe, sharp chest pain which can radiate to the arms, back, neck or jaw. In addition, you may experience: Rapid pulse. The heart compensates by beating fast in order to supply sufficient blood to the body. As a result, your pulse rises. Bloody cough. A clot can irritate your lungs, causing bleeding. You may cough up blood. Shortness of breath. A clot can block the passage of air in your lungs, leading to difficulty breathing.
Understanding the Causes of Blood Clots
Consider the danger of prolonged immobility. Blood clots sometimes form for no discernible reason, but certain conditions and situations increase your risk. The first of these is prolonged immobility. If you are on bed rest or sit and cross your legs for a long period of time, you may increase the risk of blood clots forming, particularly in your arms and legs. Extended travel in an airplane or car can minimize muscle movement, increasing the risk of blood clots forming in the veins.
Be aware of the increased risk associated with pregnancy and the postpartum period. In pregnant people, the growing uterus slows the blood flow circling back to the heart. This can increase the risk of a blood clot forming, especially in the legs or pelvis. Those who have delivered babies very recently remain at an increased risk.

Know that dehydration can cause clots. You need sufficient water in your body to make blood circulation effective. If you become dehydrated, your blood can become thicker, making it easier for clots to form.
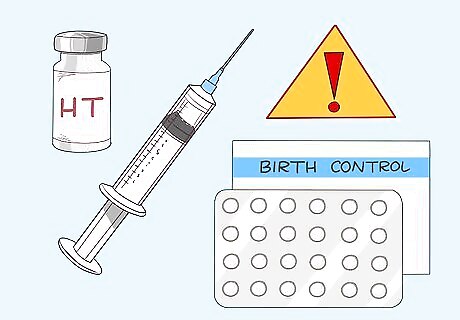
Recognize the risks of birth control and hormone therapy. Estrogen and progesterone can increase clotting factors, leading to an increased risk of clots. Hormonal contraception (like the birth control pill) and hormone therapy both introduce these hormones into the body.

Understand that long-term intravenous catheter use can lead to clots. Intravenous catheters are foreign bodies. When one is inserted into a vein, it can affect your blood circulation, leading to a clot.
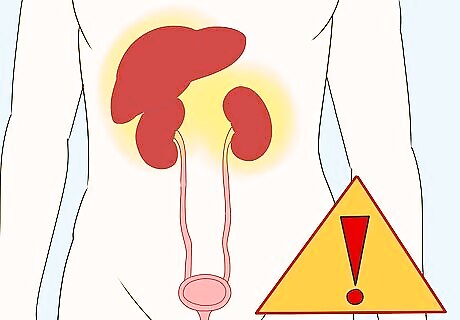
Remember that certain medical conditions can lead to clots. Certain conditions can irritate the bladder lining, causing bleeding and the development of clots, which can be passed through the urine. These conditions include: Cancer. Liver disease. Kidney disease.
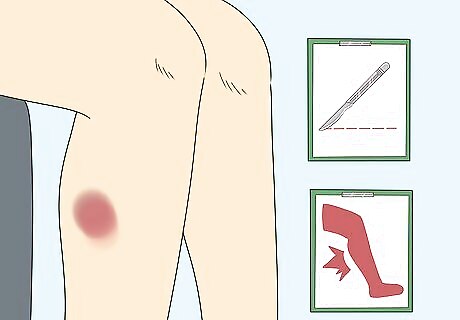
Consider the role of recent surgeries and injuries. When the body is hurt, either by an accidental injury or by a surgical procedure, excessive bleeding (and clotting) can result. In addition, the extended period of rest that usually follows surgeries and injuries increases the risk of a clot forming.

Know that obesity increases your risk. People who are significantly overweight or obese often have a buildup of cholesterol in the body. As a result, the arteries narrow, causing the formation of blood clots.

Recognize the danger of smoking. Smoking causes plaque to form in the blood vessels, narrowing them and leading to clots.
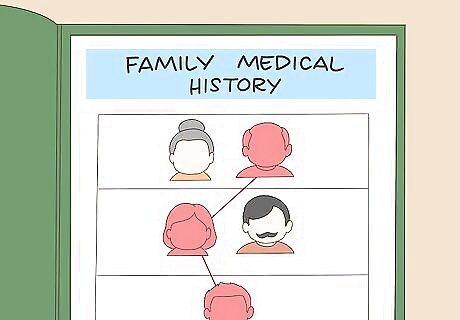
Be aware of your family history. If you have a personal or family history of clotting disorders, you are at an increased risk of developing clots. A clotting disorder may cause the blood vessels to narrow or levels of natural anticoagulants may be low, in both cases leading to blood clots.
Diagnosing Blood Clots
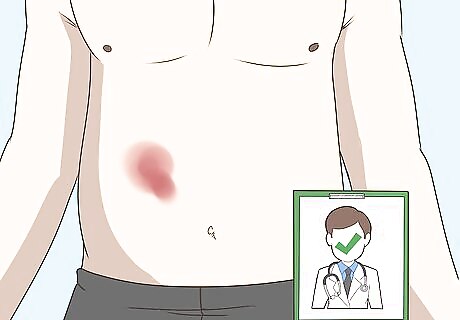
Seek medical treatment immediately. If you have any symptoms of a blood clot, get medical help right away. Blood clots can lead to life-threatening medical conditions.
Give your doctor a complete health history. Your doctor should ask questions about your symptoms, your lifestyle, your personal health history, and your family health history. Answer these questions in as much detail as possible to increase the chances of a quick and accurate diagnosis.
Have a physical exam. Your doctor should perform a complete physical, looking for any signs or symptoms that could point to blood clots.
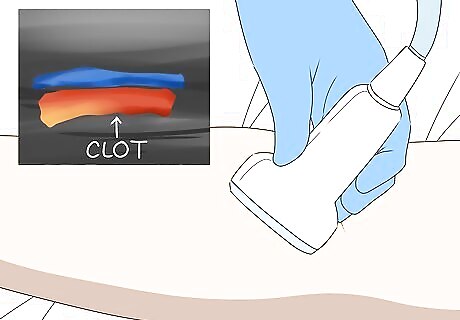
Comply with any laboratory tests your doctor orders. Depending on your symptoms, your doctor will likely order standard blood work, as well as tests that can help detect blood clotting. In addition, he or she may recommend: Ultrasound. Using an ultrasound machine, your doctor may be able to detect the formation of blood clots in the veins. Venography. In venography, a contrast dye is injected into a small vein in your hand or foot. Using fluoroscopy, the doctor can then observe the path of the dye, looking for possible clots. Arteriography. In arteriography, a dye is injected directly into an artery. Similar to venography, arteriography will allow your doctor to observe the path of the dye and confirm the presence of a clot.

Get imaging tests or ventilation perfusion to diagnose a blood clot in the lungs. If your doctor suspects a blood clot in your lungs (also known as a pulmonary embolism), he or she will recommend an imaging test and/or ventilation perfusion to check your lungs. Imaging tests can also used to see clots in the brain or in the carotid arteries. This may involve: Chest x-rays. X-rays cannot detect the presence of clots. However, they can reveal some conditions, triggered by clots, that lead to chest pain and shortness of breath. Electrocardiogram (EKG). An EKG is a painless test. It simply records your heart’s electrical activity, revealing abnormalities associated with a pulmonary embolism. Computerized tomography (CT) scan. In a CT scan, a contrast dye is injected into a vein, and your lungs or brain are scanned for signs of clots. Cerebral Angiography. This test involves a catheter, x-ray imaging and an injected contrast dye to get clear images of blood vessels in the brain. Carotid Ultrasound. This painless test images the carotid arteries with sound waves to look for blockages or narrowing, which can increase the risk of a stroke. Ventilation perfusion. Ventilation perfusion is a test in which a chemical is used to identify air inhaled into the lungs. This is then compared with the blood flow in the arteries to reveal the presence of a pulmonary embolism.
Get a specific diagnosis. Once all of the appropriate tests are performed, your doctor should be able to diagnose you with a certain type of clot. Treatment will depend, to some extent, on the type and location of your clot. Major types of clots include: Thrombus. A thrombus is a blood clot that develops in the veins or arteries. Embolus. An embolus is a thrombus that has moved from the bloodstream to another location. Deep vein thrombosis (DVT). DVT is a common and dangerous clot, usually formed in a major vein in the leg (though sometimes also appearing in the arms, pelvis, or other parts of the body). It blocks blood flow and causes pain and swelling.
Treating Blood Clots Medically

Start treatment immediately. Blood clots are life threatening, so medical action must be taken to dissolve them as quickly as possible.
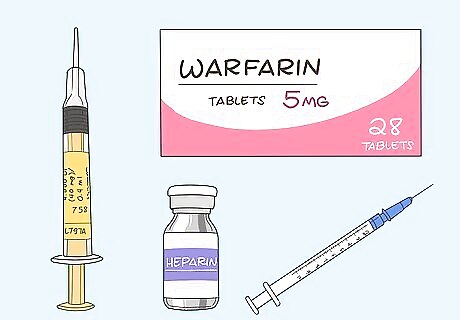
Take anticoagulants. Anticoagulant medications interrupt the process of clot formation. There are several different types on the market, including: Enoxaparin (Lovenox). Enoxaparin is a medication injected to thin the blood immediately. The typical dose for adults is 40 mg injected into a fatty area of the body, such as the arm or abdomen. Warfarin (Coumadin). Warfarin is an anticoagulation pill, which acts as a blood thinner. The dosage depends on the particular patient. To determine the dosage and administration, your doctor may perform a test for blood clotting known as the International Normalized Ratio, or INR. Heparin. Heparin is a traditional anticoagulant medication, given intravenously to prevent the growth of blood clots. The dose depends on your particular circumstances; your doctor should perform blood test measurements to determine dosage.
Talk to your doctor about thrombolytic drugs. Thrombolytic drugs, also known as “clot busters,” dissolve the fibrin strands that hold clots together. Dosage varies depending on your particular circumstances and on hospital protocols. Talk to your doctor about the right dosage for you.
Consider surgery. If medication alone cannot eliminate the clot, you will need surgery. There are a few types of surgeries that might apply: Cardiac catheterization. For blood clots in the heart, cardiac catheterization is performed to locate the clot. A balloon is inserted to open the blockage, and then a stent is placed to keep the appropriate vessel open. The pressure from the balloon and the stent breaks the blood clot into smaller pieces, restoring the flow of blood. Catheter-directed thrombolysis. A catheter-directed thrombolysis is a surgical procedure in which a catheter is inserted directly to the blood clot, releasing medication to dissolve it. Thrombectomy. A thrombectomy is simply the surgical removal of the blood clot itself. It is often performed with thrombolysis is ineffective, or when there is an emergency condition requiring immediate treatment.
Making Diet and Lifestyle Modifications

Exercise for at least 30 to 45 minutes per day. Studies suggest that regular aerobic exercise can prevent and reverse blood clot formation by increasing blood flow. Try walking, cycling, rowing, running, swimming, or jumping rope, whatever gets you moving every day. Check with your doctor about what kind of exercise is safest for you.

Drink lots of water. Dehydration thickens your blood and may lead to complications. Be sure to drink plenty of water, as staying hydrated can prevent clots from forming.
Eat foods rich in nattokinase. Nattokinase is an enzyme that breaks down fibrin, which may prevent clots from forming and dissolve those that have begun to form. Nattokinase is found in natto (a fermented Japanese food made from soybeans), fermented black beans, fermented shrimp paste, and tempeh.
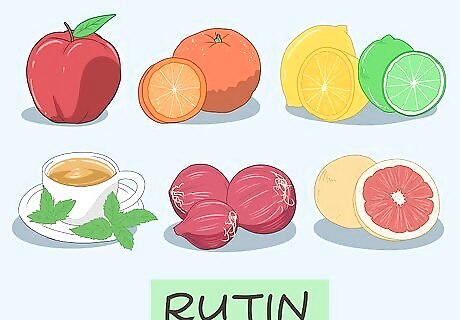
Add foods rich in rutin. Rutin targets protein disulfide isomerase, an enzyme involved in blood clotting. It is found in apples, oranges, lemons, grapefruits (note that grapefruit interacts with some blood thinners), limes, buckwheat, onion, and tea. Have one of these fruits as dessert after each meal, or incorporate them into the meals themselves.
Get plenty of bromelain. Bromelain interacts with fibrinogen to help clear away the fibrin that holds blood clots together. Bromelain is found only in pineapples. If you are at an increased risk for blood clots, considering including pineapples in your dessert after as many meals as possible.
Incorporate garlic into your diet. Garlic inhibits the production of thromboxane, which is involved in blood clots. It also contains ajoene and adenosine, which helps prevent and dissolve blood clots. Onions also include adenosine, so you should incorporate them into your diet as well.
Focus on fish for your protein servings. Too much protein (especially red meat and dairy products) seems to stimulate blood clot formation. Try to eat plenty of fish instead. The omega-3 fatty acids may reduce your cholesterol, thin your blood, and reduce clotting, though current evidence is inconclusive. For best results, focus on salmon, tuna, herring, mackerel, and sardines.

















Comments
0 comment