views
Assessing Throat and Mouth Symptoms
Determine how severe your throat pain is. Severe throat pain is usually the first sign of strep throat. You may still have strep throat even if you are only experiencing moderate throat pain, but a mild sore throat that is easily remedied or soothed is not likely to be caused by strep. The soreness should not be dependent on anything such as talking or swallowing. Soreness that can be dulled with pain medication or partially soothed with cold liquid and food might still be related to strep throat, but it is usually quite difficult to rid yourself of the soreness completely without prescription medication.
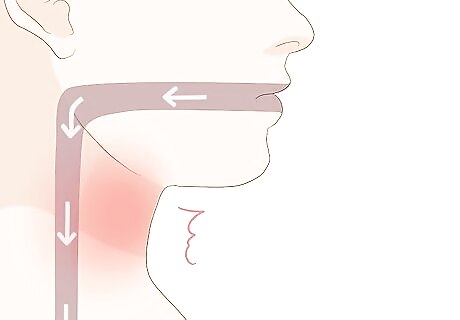
Try swallowing. If your throat is only moderately sore but becomes very painful when you swallow, you may have strep. Pain during swallowing that makes it difficult to swallow is especially common in people suffering from strep throat.

Smell your breath. While bad breath does not occur in all patients, the infection caused by streptococcus bacteria can often cause notably bad breath. This occurs as a result of the reproduction of the bacteria. While potent, the exact smell can be difficult to describe. Some state that it smells like metal or hospitals, while others compare it to rotten meat. Regardless of the exact odor, "strep breath" will smell stronger and worse than normal bad breath. Due to the somewhat subjective nature of “bad breath,” this is not really a way to diagnose strep throat, but rather a commonly seen association.
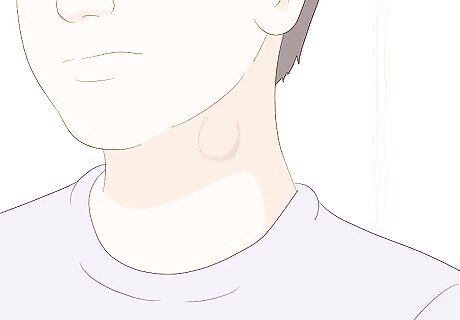
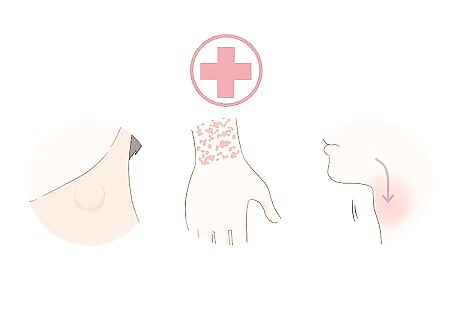
Feel the glands in your neck. Lymph nodes trap and destroy germs. The lymph nodes in your neck will usually be swollen and tender to the touch if you have strep throat. While lymph nodes are located in various parts of your body, the first nodes to swell are usually those that are nearest to the source of infection. In the case of strep throat, the lymph nodes in and around your throat will be the ones to swell. Use your fingertips to gently feel the area directly in front of your ear. Move your fingertips in a circular motion behind your ear. Also check the area of your throat just below the chin. The most common site of lymph node swelling with strep throat is under your jaw, about midway between your chin and your ear. Move your fingertips back and up toward the ear, then down the side of the neck below the ear. Finish by checking the collarbone and repeating on both sides. If you can feel notable swelling or bulging in any of these areas, your lymph nodes might be swollen due to strep.
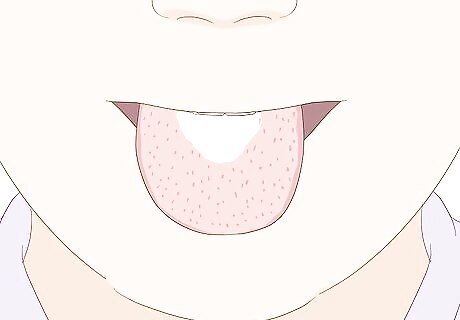
Check your tongue. People with strep throat often have a prickly coating of tiny red dots along their tongue, especially toward the back of the mouth. Most people compare this prickly coating to the outside of a strawberry. These red dots can either be bright red or dark red. They generally appear to be inflamed.
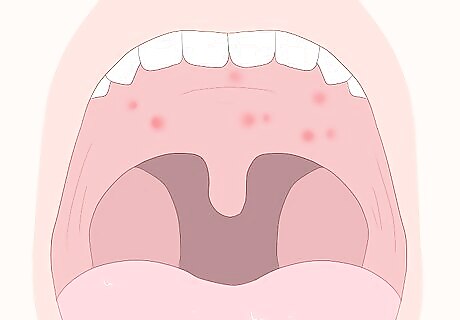
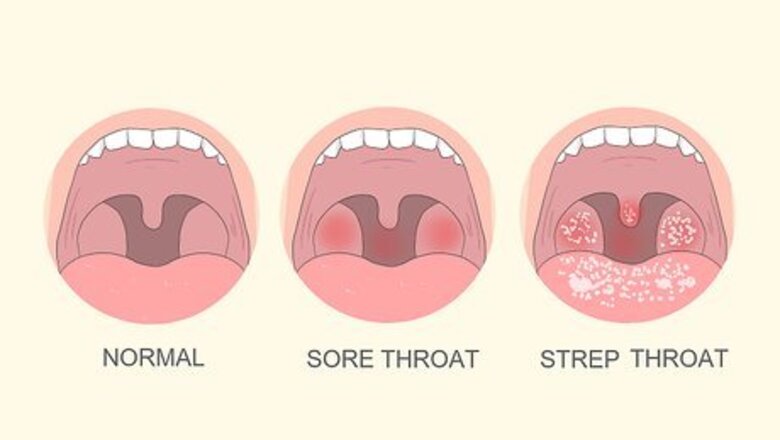
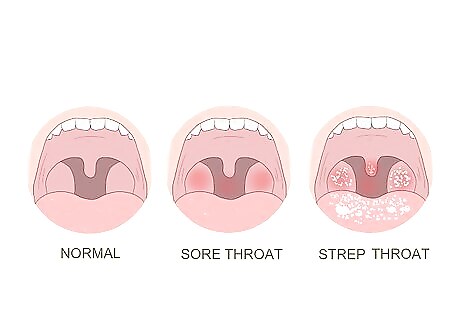
Check the back of your throat. Many who suffer from strep throat develop petechiae, red spots on the soft or hard palate (on the roof of the mouth, near the back).
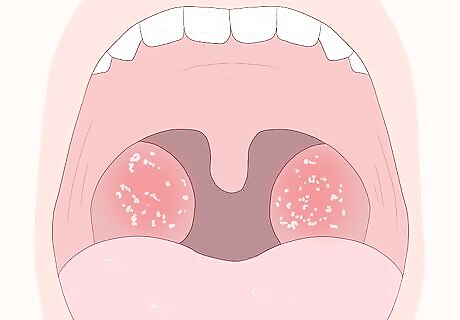
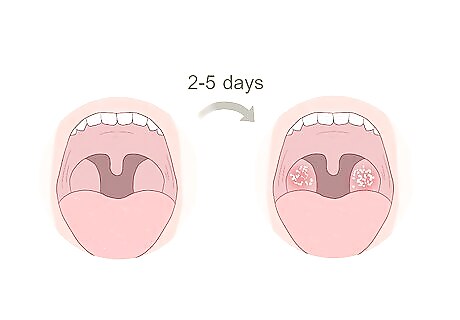
Check your tonsils if you still have them. Strep throat will usually cause your tonsils to become inflamed. They will appear a brighter or deeper red than usual and will be notably enlarged. You may also notice that the tonsils are coated in patches of white. These patches of white can be located directly on the tonsils or simply in the back of the throat. They can also appear yellow instead of white. Instead of white patches, you may notice long streaks of white pus coating your tonsils. This is also a symptom of strep throat.
Assessing Other Common Symptoms
Note if you have been around someone with strep throat. The infection is contagious and is spread through direct contact with the bacteria that causes it. It is unlikely that you will develop strep throat without having had direct contact with someone who is infected. It can be very difficult to know if someone else has strep. Unless you have been isolated completely, you probably could have come in contact with someone who has the infection. It is also possible for individuals to carry and pass on strep without having symptoms themselves.
Consider how quickly the illness came on. A sore throat associated with streptococcus usually develops without warning and worsens very quickly. If your throat became increasingly sore over the course of several days, another cause is most likely to blame. However, this alone does not rule out strep throat.
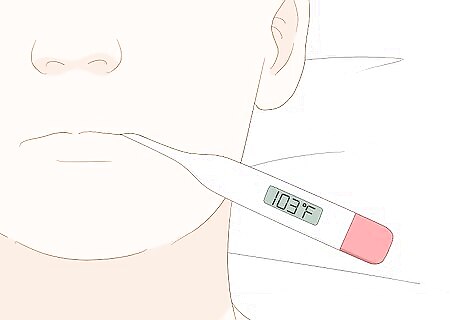
Check your temperature. Strep throat is usually accompanied by a fever of 101 degrees Fahrenheit (38.3 degrees Celsius) or higher. A lower fever could still be caused by strep, but it is more likely to be a symptom of a viral infection.
Pay attention to any headaches. Headaches are another common symptom of strep throat. They can range in severity from mild to excruciating.
Monitor any digestive symptoms. If you lose your appetite or feel nauseous, you can count that as another possible symptom of strep throat. At its worst, strep throat can even lead to vomiting and stomach pain.
Take fatigue into account. As with any infection, strep throat can lead to increased fatigue. You may find it harder to wake up in the morning than usual and harder to make it through the day.

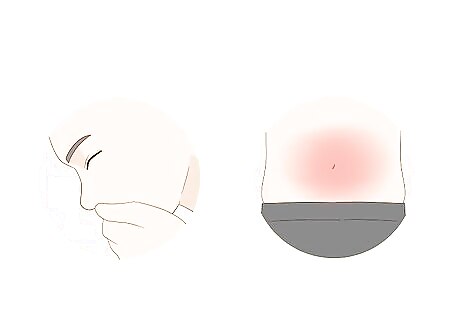
Look for a rash. Severe strep throat infections can cause a condition known as scarlatina, more commonly referred to as scarlet fever. This red rash will look and feel very similar to sandpaper. Scarlet fever usually surfaces 12 to 48 hours after your first strep throat symptoms emerge. The rash usually begins around the neck before developing and spreading over the chest. It can also spread to the abdomen and groin areas. In rare cases, it may appear on the back, arms, legs, or face. When treated with antibiotics, scarlet fever generally clears up quickly. If you notice a rash of this nature, you should visit the doctor as soon as possible, regardless of whether or not other strep throat symptoms are present.
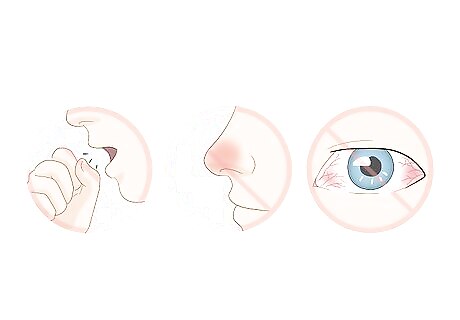
Note any absent symptoms. While colds and strep throat share many symptoms, there are several cold-like symptoms that people with strep throat tend not to display. The absence of these symptoms can be another sign that you have strep throat, rather than a cold. Strep throat does not usually cause nasal symptoms. This means that you will not experience a cough, runny nose, stuffy nose, or red, itchy eyes. Additionally, while strep throat can cause stomach pain, it does not usually cause diarrhea.
Assessing Your Recent History and Risk Factors
Examine your medical history. Some people seem to be more prone to developing strep infections than others. If you have a history of strep infections, it is more likely that a new infection could also be strep.
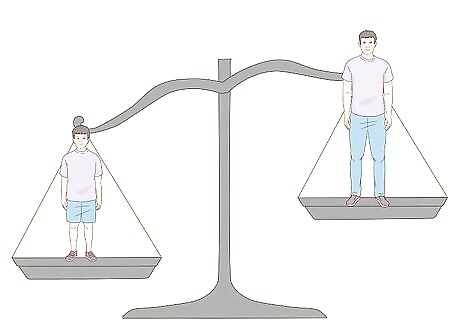
Assess whether your age makes it likely that you have contracted strep throat. While 20%-30% of sore throats in children are due to strep throat, only 5%-15% of sore throat visits to the doctor by adults are due to strep throat. Elderly patients, as well as individuals with concurrent illness (such as the flu), are more susceptible to opportunistic infections.
Figure out if your living situation increases your risk of strep throat. There is often a higher likelihood of strep throat when other family members have had strep throat in the past two weeks. Shared indoor living or play spaces such as schools, daycares, dormitories, and military barracks, are examples of environments that pose a potential for colonization of bacteria. While children are at higher risk for strep throat, babies under age 2 are much less likely to be infected with strep throat. However, they may not have the usual symptoms as older children and adults. They may have a fever, runny nose, or cough as well as a decreased appetite. Ask your doctor about your baby's risk of getting strep throat if you or another close contact has strep and they have a fever or other symptoms.

Assess whether you have any health risk factors that might make more susceptible to strep throat. Immunocompromised individuals, those with the decreased ability to fight off infection, may be more at risk. Other infections or illnesses can also increase the chances that you have strep. Your immune system may be compromised simply due to fatigue. States of extreme exertion or exercise (such as running a marathon) can also tax your body. As your body focuses on recovery, it’s ability to fight infection may be impeded. Simply put, an exhausted body is focused on recovery and may not be able to defend itself as efficiently. Smoking can cause damage to your protective mucosa in the mouth and allow for easier colonization of bacteria. Oral Sex can expose your oral cavity to be more directly exposed to bacteria. Diabetes decreases the ability of your body to fight infection.
Visiting the Doctor
Know when to see a doctor. While you don't need to see the doctor every time a sore throat pops up, some potential strep throat symptoms should cause you to make an appointment right away. If your sore throat is accompanied by swollen lymph nodes, a rash, difficulty swallowing or breathing, a high fever, or a fever lasting more than 48 hours, call the doctor for an appointment. You should also talk to your doctor if your sore throat lasts longer than 48 hours.
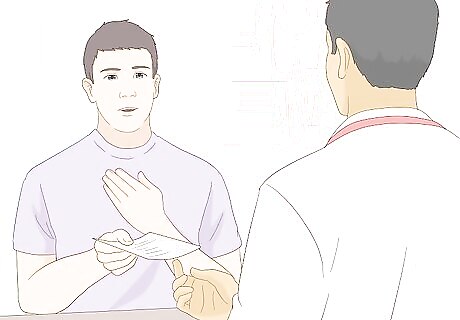
Let the doctor know about your concerns. Bring the doctor a thorough list of your symptoms and let them know that you suspect strep might be to blame. Your doctor will usually check for some of the most telling signs of the disease. Expect your doctor to take your temperature. Also expect your doctor to look inside your throat with a light. He or she will most likely want to check for swollen tonsils, a red bumpy tongue rash, or white or yellow spots in the back of the throat.
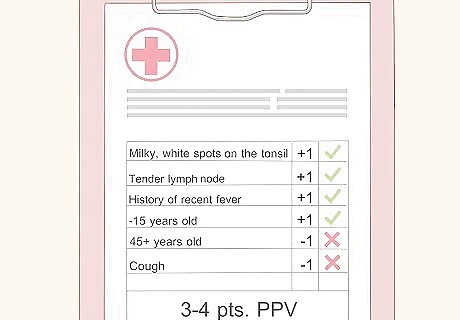
Expect your doctor to go through a clinical diagnosis protocol. This protocol is basically an organized way for your doctor to assess your symptoms. For adults, your doctor may use what is known as a Modified Centor Clinical Prediction Rule in order to empirically indicate how likely it is that you have a group A Streptococcal infection. This is simply a list of criteria that the doctor checks for to determine whether (and how) you should be treated for strep throat. The doctor will tally points, positive or negative, for signs and symptoms: +1 point for milky, white spots on the tonsils (tonsillar exudates), +1 point for tender lymph nodes (tender anterior chain cervical adenopathy), +1 point for a history of recent fever, +1 point for less than 15 years of age, +0 point for an age between 15-45 years old, -1 point for being greater than 45 years old, and -1 point for a cough. If you score 3-4 points, then there is a positive predictive value (PPV) of roughly 80% that you have a group A streptococcal infection. Basically, you are considered positive for strep. This infection should be treated with antibiotics and your doctor will prescribe the proper regimen.
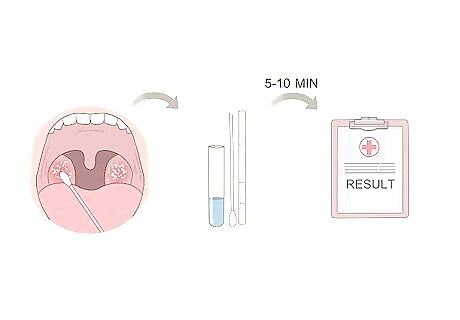
Ask the doctor for a rapid strep test. The Centor criteria has not proven effective in predicting antibiotic treatment-worthy infection in children. A rapid strep antigen test may be performed in the office and only takes a few minutes to complete. The doctor will use a cotton swab (similar to a Q-tip) to sample the fluids in the back of your throat for bacteria. These fluids will then be tested in the office, and within 5 to 10 minutes, you should know the results.
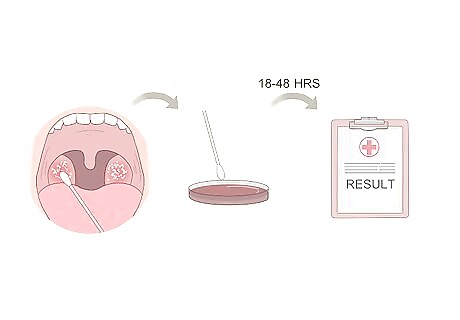
Ask the doctor for a throat culture. If the results of your rapid strep test are negative but you still exhibit other strep throat symptoms, the doctor may want to administer a longer test known as a throat culture. A throat culture will attempt to colonize bacteria outside of your throat in a lab. As the bacteria colony collected from your throat grows, it will become easier to detect larger amounts of group A streptococcus bacteria. Your doctor will likely use any combination of the Centor criteria, rapid strep test, and throat culture, depending on his or her clinical judgment. While rapid strep tests alone are usually enough to determine whether or not a strep infection is present, false-negatives have been known to occur. Throat cultures, by comparison, are more accurate. A throat culture is not needed if the rapid strep test comes back positive, as the rapid strep test directly tests for antigens to the bacteria and will only test positive if a threshold level of bacteria are present. This would indicate immediate treatment with antibiotics. The doctor will use a cotton swab to collect a sample of fluids from the back of your throat. The doctor will send the swab to a lab and the lab will transfer that sample to an agar plate. The plate will incubate for 18-48 hours depending on the methodology of the specific lab. If you have strep throat, then Beta Streptococcus Group A bacteria will grow in the dish.
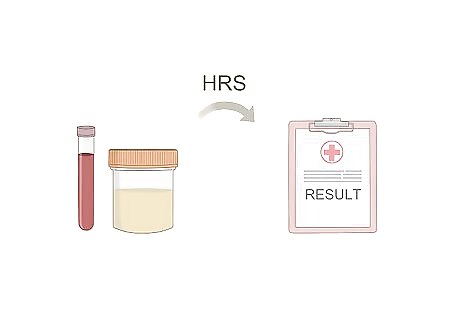
Find out about other testing options. Some doctors prefer a nucleic acid amplification test (NAAT) instead of a throat culture for negative rapid tests. This test is accurate and shows a result in a matter of hours, instead of requiring 1-2 days of incubation.
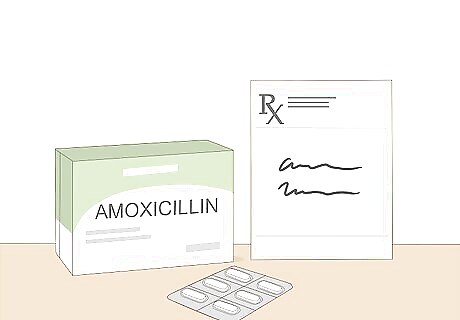
Take your antibiotics if prescribed by your doctor. Strep throat is a bacterial infection and, as such, is treated effectively with antibiotics. If you have any known allergies to antibiotics (such as penicillin), it is important to let your doctor know so he or she can provide you with appropriate alternatives. A typical course of antibiotics is usually up to 10 days (depending on specific antibiotics decided by your doctor). Be sure to take your antibiotics for the fully prescribed time, even if you feel better before you finish the full course. Penicillin, Amoxicillin, cephalosporins, and Azithromycin are all common antibiotics that can be used to treat an infection. Penicillin is used often and effectively in the treatment of Strep throat. However, some individuals may have allergic reactions to this medication. You should let your doctor know if you are aware of this possible side effect. Amoxicillin is another drug of choice for strep throat with good results. It is similar to penicillin in effectiveness and can withstand the gastric acid in your stomach better before being absorbed into your system. Additionally, it has a broader activity spectrum than penicillin. Azithromycin, Erythromycin, or cephalosporins are used as an alternative to Penicillin when a person is known to have allergies to penicillin. Note that erythromycin has higher rates of gastrointestinal side effects in people.
Stay comfortable and rest while the antibiotics take effect. The typical recovery should take about as long as you take antibiotics (up to 10 days). While you are healing, give your body the opportunity to recover. Extra sleep, herbal teas, and plenty of fluids can help alleviate throat pain while you recover. In addition, it is sometimes helpful to consume cold beverages, ice cream, and popsicles to ease throat pain.
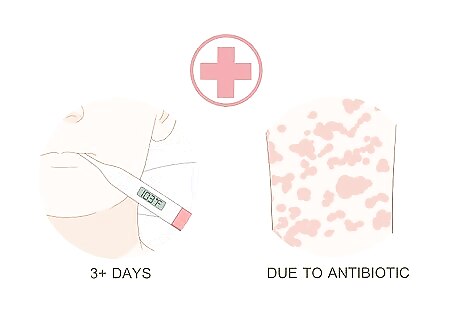
Follow up with your doctor if you need to. You should feel better in 2-3 days; if you do not, or if you still have a fever, call your doctor. Additionally, if you show any signs of an allergic reaction to the antibiotics, call your doctor immediately. Signs of a reaction include a rash, hives, or swelling after taking an antibiotic.



















Comments
0 comment