
views
X
Expert Source
Lydia Shedlofsky, DODermatologist
Expert Interview. 11 November 2020.
It's most common in children who have weakened immune systems, but adults can get it too — it's considered a sexually transmitted infection (STI) when it involves the genitals. Molluscum contagiosum often goes away on its own, but recognizing common symptoms can lead to helpful treatment and prevent confusing it for other, more serious conditions.
Recognizing Symptoms of Molluscum Contagiosum

Know who's at risk. Molluscum contagiosum is common enough that you probably know someone who's had it. It's not limited to kids, but it's most common in children between the ages of 1 to 10 years who have weakened immunity due to poor nutrition or other illnesses. Other people at increased risk for the skin infection include chemotherapy patients, the elderly and people infected with HIV. Having atopic dermatitis (allergic skin reactions) may also put you at higher risk of developing molluscum contagiosum. Participation in contact sports is a risk factor for molluscum contagiosum. In general, molluscum contagiosum infections are more common in warm, humid climates where people live crowded together, such as India and parts of Asia.
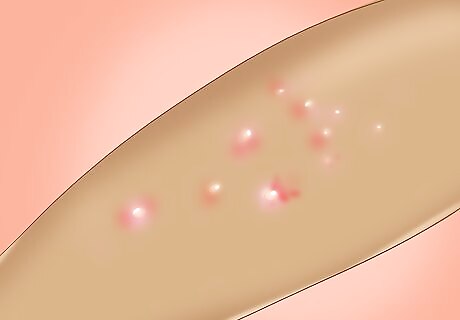
Watch for round, raised lesions. The lesions or bumps characteristic of molluscum contagiosum are typically small, round and raised above the surface of the skin. Most people get between 10 – 20 bumps on their skin, but people with AIDS can develop 100 or more bumps. In terms of color, they are usually whitish, pink or flesh-colored. The raised bumps range in size from about 2 – 5 mm millimeters in diameter (about the size of a tip of a crayon to the size of a pencil eraser), although they can get bigger around the genitalia of adults. These bumps can appear anywhere on the body, but are usually seen on the face, neck, armpit, arms and hands. The only places they will not appear are the palms of the hands and soles of the feet. They appear about seven weeks after being exposed to the virus. The fleshy lesions are known as mollusca and can sometimes mimic warts, heat blisters and other benign growths such as skin tags.
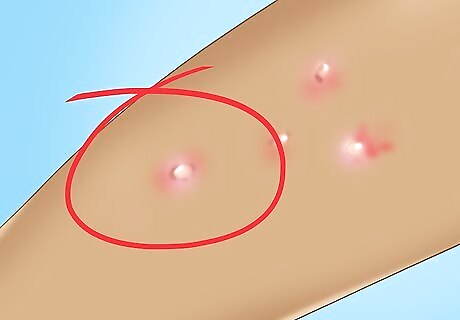
Take notice if the bumps get red and inflamed. Normally the lesions or bumps (mollusca) are not particularly itchy, although that can change if you scratch them. By scratching, itching or rubbing the lesions, you can make them red, inflamed and itchy, which increases the likelihood that they'll spread to surrounding skin and make the condition worse. Mollusca can easily be removed by scratching, rubbing, or even just casual contact, unlike pimples, warts and other skin lesions. Mollusca that have turned red and inflamed without any scratching is usually a sign that your immune system has regained enough strength to fight the infection. Once red and inflamed, mollusca can look a lot like regular pimples, ingrown hairs or even chicken pox. Inflamed lesions should not be confused for infection and do not need antibiotics.

Look for a small indentation. Mollusca can often be identified from other skin lesions and blemishes because they have a characteristic indentation, dimple, or pit in their center that's called an umbilication. This central umbilication may be filled with a thick, white substance that is cheesy or waxy looking. The material can be squeezed out, but it makes the infection much more contagious, so don't pick at them. The umbilication can sometimes make mollusca look like blackhead pimples or pustules (whiteheads). The waxy or cheesy material inside of the mollusca contain millions of viruses mixed with your skin's oily secretions and often some pus, which is dead white blood cells.
Preventing Molluscum Contagiosum
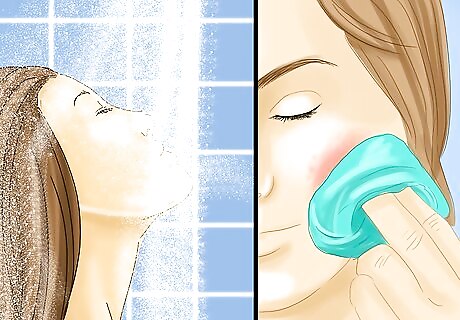
Practice good hygiene. Practicing good hygiene is an effective way of avoiding or preventing many different kinds of infections, including molluscum contagiosum; therefore, wash your hands frequently with warm water and soap, especially if you shake hands or touch someone with visible lesions on their body. Hand washing also removes viruses (and other germs) that you pick up from contaminated surfaces, toys, clothing or towels. After bathing your body, don't be too aggressive while drying it. Pat yourself with the towel gently instead of rubbing because you don't want to remove the mollusca and make the skin infection more contagious. In addition to washing your hands, try to stop the habit of putting your hands into your mouth or rubbing your eyes — it'll help prevent infection also. An alcohol-based hand sanitizer is also effective against molluscum contagiosum and can be used as a good alternative to soap and water. Infection can spread via bath sponges, towels, pumice stones, or razors. Avoid sharing these items.

Avoid sexual contact. The viral infection also spreads by sexual contact among teens and adults because the lesions can develop on and around the genitals of both genders (upper thighs and lower abdomen are common locations also). Practicing safe sex (with a condom) is not enough to prevent molluscum contagiosum because it's spread by skin-to-skin contact, not in body fluids. The best practice is to completely avoid sexual contact if you or your partner have mollusca near the genitalia until the condition completely goes away. Oral sex also needs to be avoided if you or your partner have mollusca near the mouth or on the face. Mollusca on the genitalia are often mistaken for genital herpes, but they don't cause the burning pain of herpes.

Don't scratch the bumps. As difficult as it may be, particularly if they've become inflamed and itchy, you should avoid scratching, rubbing or even touching the mollusca lesions. Picking or scratching your skin can spread the virus to other parts of your body and make it easier to spread the infection to others. Be particularly careful about not scratching around your eyes because you increase the risk of an eye infection (conjunctivitis). Shaving over the infected areas can also disrupt or remove the mollusca and spread the virus. As such, avoid shaving your face, underarms or legs if you have lesions in those locations.
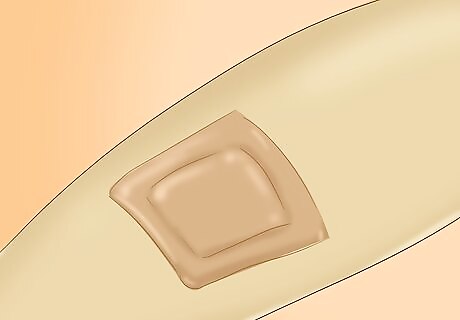
Keep molluscum lesions covered. If you are already infected with molluscum contagiosum, then the best way to prevent spreading it to other parts of your body or to other people is to keep the infected area covered with loose breathable clothing or light bandaging. The physical barrier will prevent you from scratching and keep others from touching the mollusca. Remember to always keep the infected skin clean and dry beneath the clothes or bandages. Use watertight bandages to cover your bumps and change them regularly (daily if you get them wet). Wearing loose cotton clothing is a much better choice than thicker wool or synthetic fibers that aren't breathable.
Treating Molluscum Contagiosum

Wait and see. Molluscum contagiosum is self-limiting and eventually fades away in healthy individuals, so treatment is often unnecessary. It usually takes between six to 12 months for the infection to resolve and the mollusca to disappear. In some immune-weakened people, it may take up to five years for all the bumps to disappear on their own. Treatment is sometimes recommended by doctors if the bumps are in the genital area.
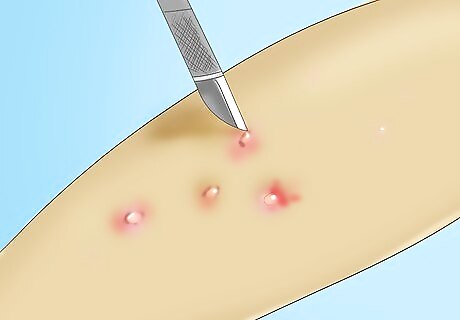
Get the bumps/lesions removed. Sometimes doctors may recommend the lesions be surgically removed before they disappear on their own (often in adults) because they tend to be so contagious and people are often self-conscious or embarrassed by them. This is particularly true if the mollusca are on or near the penis, vulva, vagina or anus. Ask your doctor if your situation is appropriate for removal. Surgical removal can include cryotherapy (freezing with liquid nitrogen), curettage (scraping away the lesion) and laser therapy. These removal methods are usually painful and require local anesthesia. Scarring is not uncommon with these procedures. Your doctor might attempt to remove your mollusca, but often they will refer you to a skin specialist (dermatologist).
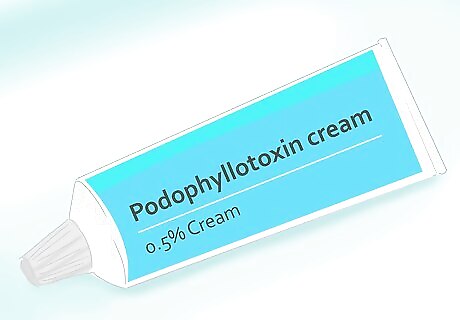
Try medications. In some cases, prescription creams or ointments applied directly to the mollusca may be helpful and get rid of them quicker. Common examples include tretinoin (Atralin, Retin-A), adapalene (Differin), tazarotene (Avage, Tazorac) and imiquimod. Be aware that these topical drugs cannot be used during pregnancy due to risk of side effects to the unborn baby. Sometimes preparations containing salicylic acid or potassium hydroxide are used for molluscum contagiosum — they help dissolve lesions by causing blisters to form over them. Podophyllotoxin cream or podofilox may be helpful as an over-the-counter therapy to use at home. In one study patients applied 0.5% cream twice a day for three consecutive days a week, versus a group applying a placebo. Treatment was continued for four weeks. After four weeks, 92% of the 0.5% podofilox group was cured. Remember to apply this cream liberally to the affected area.


















Comments
0 comment