views
X
Trustworthy Source
National Institute of Diabetes and Digestive and Kidney Diseases
Health information from the National Institute of Diabetes and Digestive and Kidney Diseases, a division of the U.S. National Institutes of Health
Go to source
Research suggests that cirrhosis of the liver usually can't be reversed, though you may be able to slow the progress of the condition. Since symptoms may not show until your liver is already seriously damaged, see your doctor right away if you suspect you may have cirrhosis so you can start treatment if necessary.[2]
X
Trustworthy Source
Mayo Clinic
Educational website from one of the world's leading hospitals
Go to source
Understanding the Risk Factors
Think about how much alcohol you drink. Alcohol damages the liver by blocking its ability to process carbohydrates, fats, and proteins. When these things build up in damaging levels in the liver, the body may react with reactive inflammation that leads to hepatitis, fibrosis, and cirrhosis. However, excessive alcohol use is not sufficient to promote alcoholic liver disease. Only 1 in 5 heavy drinkers develop alcoholic hepatitis, and 1 in 4 develops cirrhosis. Men are considered "heavy drinkers" if they have 15 or more drinks in a given week. Women are considered "heavy" drinkers with 8 or more drinks per week. You can still develop cirrhosis after you've stopped drinking. However, alcohol abstinence is still recommended for all people with cirrhosis. It will help treatment and healing, no matter what stage of the disease you're in. While cirrhosis is more common in men, cirrhosis in women is more likely to result from alcoholism.
Get tested for hepatitis B and C. The chronic liver inflammation and injury from either virus can, over several decades, develop into cirrhosis. Risk factors for hepatitis B include unprotected sex, blood transfusions, and injection drug use with contaminated needles. This is a lot less prevalent in the US and other developed countries due to vaccinations. Risk factors for hepatitis C include infections from injection drug use, blood transfusions, and body piercing and tattoos. Cirrhosis from hepatitis C is the most common reason for liver transplants.
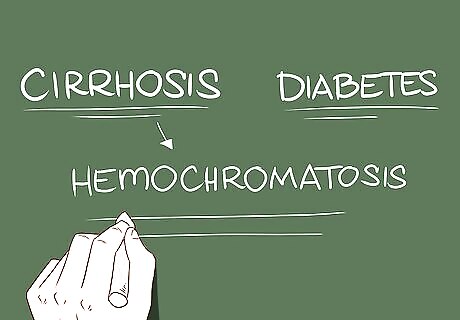
Be aware of a correlation between cirrhosis and diabetes. In 15-30% of people with cirrhosis, diabetes is a risk factor for developing "non-alcoholic steatohepatitis" (NASH). Diabetes is also common in chronic hepatitis C infections — a common cause of cirrhosis — likely because of decreased pancreas function. Another cirrhosis cause that's often correlated with diabetes is hemochromatosis. This condition is characterized by iron deposits in the skin, heart, joints, and pancreas. The pancreatic buildup leads to diabetes.
Take your current weight into account. Obesity presents a wide variety of health concerns, from type 2 diabetes and heart disease to arthritis and stroke. But, the excess fat in the liver causes inflammation and damage that could develop into non-alcoholic steatohepatitis. To determine whether you are within a healthy weight range, take advantage of an online BMI (body mass index) calculator. A BMI calculation takes into consideration your age, height, gender, and weight.
Know the risks from autoimmune and heart diseases. If you have an autoimmune disease like inflammatory bowel disease, rheumatoid arthritis, or thyroid disease, be cautious. While they don't directly contribute to cirrhosis, they increase the risk of complications in other disorders that do lead to it. Heart disease is a risk factor for non-alcoholic steatohepatitis leading to cirrhosis. Furthermore, heart disease related to right-sided heart failure can cause liver congestion (nutmeg liver) and cardiac cirrhosis.
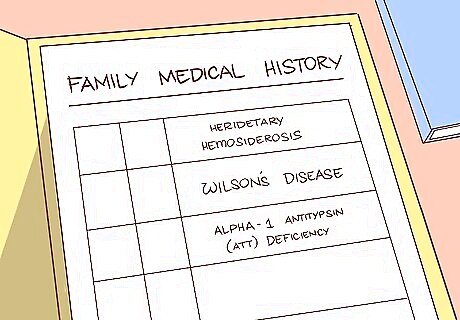
Examine your family history. Certain types of liver disease that cause cirrhosis have a pattern of genetic inheritance. Look at your family's medical history for diseases that put you at an increased risk for cirrhosis: Hereditary hemosiderosis Wilson's disease Alpha-1 antitrypsin (AAT) deficiency
Recognizing the Symptoms and Signs
Recognize the symptoms of cirrhosis. If you observe these symptoms, you should bring it to a doctor's attention as soon as possible. He or she will be able to give you a professional diagnosis and immediately begin the treatment process. If you’re trying to find out if someone other than yourself has cirrhosis, make sure to include that person in your evaluation, as there may be symptoms that can't be observed from the outside. The symptoms of cirrhosis include: Fatigue, or feeling tired Easy bruising or bleeding Lower extremity edema (swelling) Yellow-tinted skin and eyes (jaundice) Fever Lack of appetite or weight loss Nausea Diarrhea Intense itching (pruritus) Increased abdominal girth Confusion Sleep disturbance
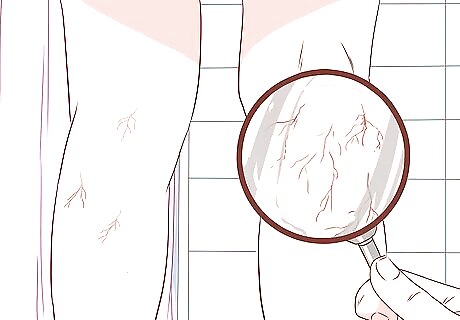
Look for spider veins. The more technical terms for this condition are spider angiomata, spider nevi, or spider telangiectasias. Spider veins are an abnormal cluster of veins that sprout from a central blood vessel with a lesion. They usually appear on the trunk of the body, the face, and the upper limbs. To verify spider veins, press a piece of glass over the suspected cluster of veins. The red dot in the center of the cluster will seem to pulsate — getting red as blood enters, then blanching as blood exits to the smaller veins. Large and multiple spider angiomas are a sign of more severe cirrhosis. However, they are also common with pregnancy and severe malnutrition. Occasionally, they are seen in otherwise healthy individuals.

Observe the palms for reddening. Palmar erythema looks like speckled patches of reddening spots on the palm, and is caused by changed sex hormone metabolism. Palmar erythema mainly affects mainly the outer edges of your palms along your thumb and pinky, and spares the central palm. Other causes of palmar erythema include pregnancy, rheumatoid arthritis, hyperthyroidism, and blood problems.
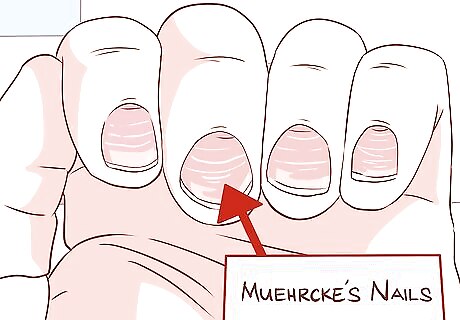
Note any changes in the nails. Liver disease in general often affects the skin, but observing the nails can provide useful additional information. Muehrcke's nails are pale horizontal bands or stripes that run across the nail bed. This is a result of inadequate production of albumin, which is solely made by the liver. Pressing on these nails will make the bands blanche and disappear before quickly returning. With Terry's nails, the two-thirds of the nail plate closest to the knuckle appears white. The one-third closer to the tip of the finger appears red. This is also due to inadequate albumin. Clubbing is a rounding and/or enlargement of the nailbed and the tip of the finger. When severe, the fingers may appear like drumstick, thus the term "drumstick fingers." This is more commonly seen with biliary cirrhosis.

Inspect long bone joints for swelling. If you see recurring swelling at the knee or ankle, for example, it may be a sign of "hypertrophic osteoarthropathy" (HOA). Joints in the fingers and shoulders may also feel arthritic. This is the result of chronic inflammation in connective tissue surrounding the bone, which can be very painful. Note that the most common cause of HOA is lung cancer, which must be ruled out.
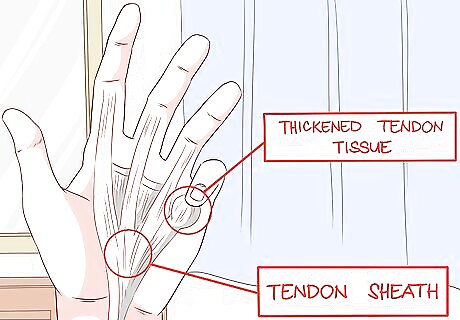
Look for curled fingers. "Dupuytren's contracture" is a thickening and shortening of palmar fascia — the tissue that connects the different parts of the palm. This leads to problems with finger flexibility, causing them to curl permanently. It's most common in the ring and pinky finger and is often accompanied by pain, aching, or itching. The person will have trouble holding objects, as the condition affects grip strength. Dupuytren's contracture is common in alcoholic cirrhosis, occurring in about one-third of cases. However, it is also seen in smokers, alcohol users without cirrhosis, workers with repetitive hand motions, and people with diabetes mellitus and Peyronie's disease.
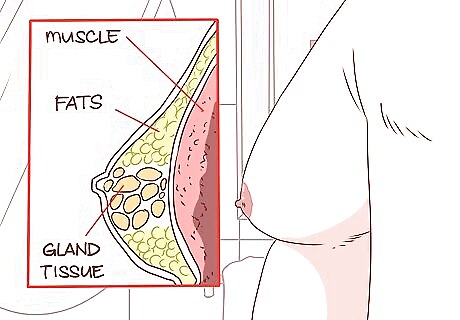
Check for a firm mass in men's breasts. Gynecomastia is a growth of gland tissue in men's breasts that extends out from the nipples. This results from an increase in the hormone estradiol and is seen in up to two-thirds of cirrhosis cases. Gynecomastia might appear like pseudogynecomastia, which breast enlargement from fat rather than glandular proliferation. To tell them apart, lie on your back and place your thumb and forefinger on each side of the breast. Slowly bring them together. You're feeling for a concentric, rubbery-to-firm disk of tissue directly under the nipple area. If you feel the mass, there is gynecomastia present.If you don't feel the mass, you have pseudogynecomastia. Other mass disorders, such as cancer, tend to be eccentrically located (not centered around the nipple).

Observe symptoms of hypogonadism in men. Men with chronic liver problems like cirrhosis see a decrease in testosterone production. Symptoms of hypogonadism include impotence, infertility, loss of sexual drive, and shrunken testicles. It may be caused by an injury to the testicle or through a problem with the hypothalamus or pituitary gland.

Take note of abdominal pain and bloating. These can be signs of ascites, a buildup of fluid in the peritoneal (abdominal) cavity. If enough fluid accumulates, you may also experience shortness of breath.
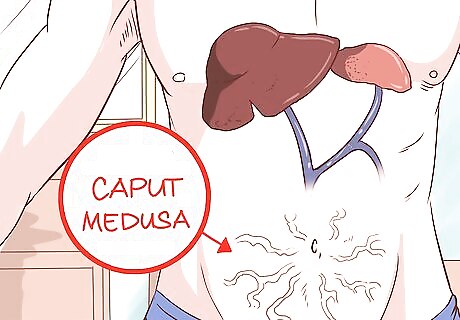
Inspect the abdomen for prominent veins. Caput medusa is a condition in which the umbilical vein opens, letting blood back up in the portal venous system. That blood is then shunted into the umbilical vein, then the abdominal wall veins. This makes veins highly visible on the stomach. This increased prominence is called caput medusa, because it resembles the head (caput) of Medusa, from Greek mythology.

Smell the breath for a musty odor. This indicates "fetor hepaticus," and is caused by severe cases of the same hypertension that causes a caput medusa and the for Cruveilhier-Baumgarten murmur. The odor comes from an increased amount of dimethyl sulfide as a result of the hypertension. The murmur grows quieter when the doctor flattens the blood vessels by applying pressure on the skin above the belly button.

Notice yellow eyes and skin. Jaundice is a condition that causes this yellowish discoloration due to increased bilirubin when the liver can't process it effectively. Mucus membranes may also become yellow, and urine may appear darkened. Now that yellow skin can also be caused by eating a lot of carotene through carrots. However, carrots will not turn the white of the eyes yellow, as jaundice will.
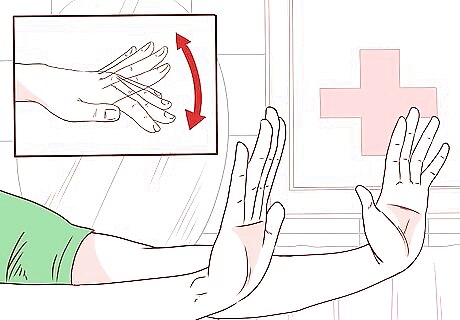
Test the hands for asterixis. Ask the person you suspect of having cirrhosis to fully extend their hands in front of them with palms flat and facedown. The individual’s hands will begin moving and “flapping” at the wrist like a bird’s wings. Asterixis is also seen in uremia and severe heart failure.
Seeking Expert Medical Diagnosis
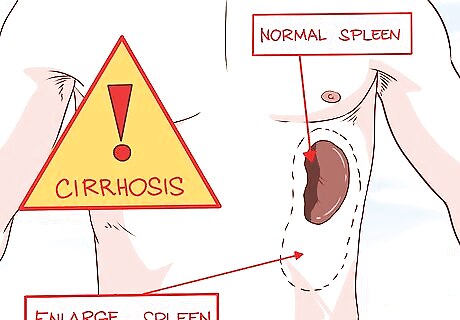
Ask a doctor to check for a change in liver or spleen size. When probed, the cirrhotic liver tends to feel firm and nodular. Splenomegaly (enlarged spleen) is caused by hypertension that causes congestion in the spleen. Both of these conditions are signs of cirrhosis.
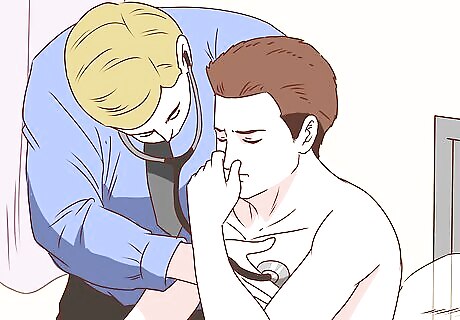
Have the doctor check for Cruveilhier-Baumgarten murmur. Most primary care doctors will not check for this. This is a hum in the veins that can be heard through a stethoscope in the epigastric (upper central) region of the abdomen. Like caput medusa, it's also caused by a problem with the way different vein systems in the body connect to one another when there's high pressure in the veins. The doctor will perform the Valsalva maneuver — a probing technique that increases abdominal pressure. This will allow him or her to hear the murmur more clearly if it is present.
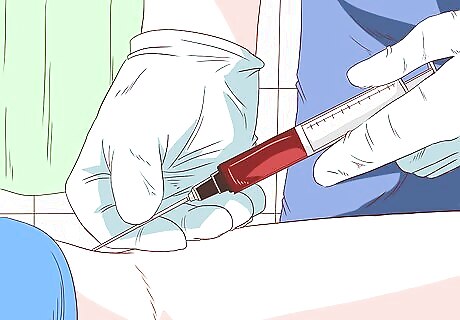
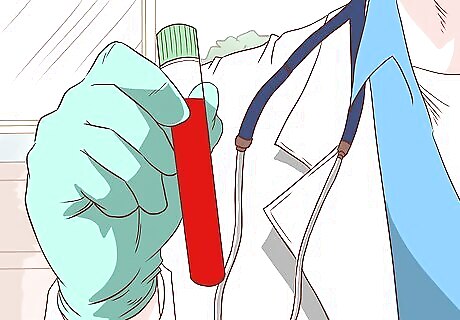
Allow the doctor to perform blood tests for cirrhosis. He or she will draw blood and have a laboratory perform tests useful for a diagnosis of cirrhosis. These tests may include: A complete blood count that tests for the anemia, leukopenia, and neutropenia, and thrombocytopenia commonly seen in cirrhosis, among other things. A test for elevated serum aminotransferases enzyme levels that might point to alcoholic cirrhosis. Alcoholic cirrhosis typically has AST/ALT ratio greater than 2. A measurement of total bilirubin to compare your levels to acceptable baseline levels. Results may be normal in early cirrhosis, but levels tend to rise as cirrhosis worsens. Note that rising bilirubin is a poor prognostic sign in primary biliary cirrhosis. A measurement of albumin levels. A failing, cirrhotic liver's inability to synthesize albumin will lead to low albumin levels. However, this is also seen in patients with congestive heart failure, nephrotic syndrome, malnutrition, and some intestinal disease. Other tests include alkaline phosphatase, gamma-glutamyl transpeptidase (GGT), prothrombin time,, globulins, serum sodium, and hyponatremia.
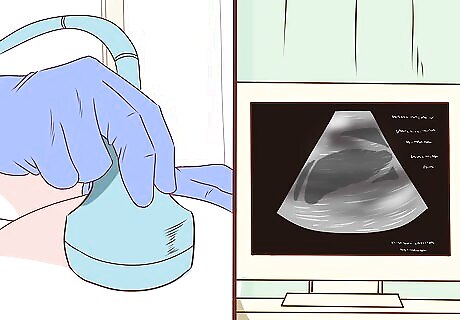
Have the doctor perform imaging studies. Imaging the body can help recognize cirrhosis, but are more useful to detect complications of cirrhosis like ascites. Ultrasounds are noninvasive and widely available. A cirrhotic liver appears small and nodular on an ultrasound. The classic finding in cirrhosis is shrinking of the right lobe and enlargement of the left one. Nodules seen on ultrasound may be benign or malignant and need to be biopsied. Ultrasounds can also detect increased portal vein diameter or the presence of collateral veins that suggest portal hypertension. Computed tomography isn't routinely done for cirrhosis, as it provides the same information as ultrasound. Furthermore, it involves radiation and contrast exposure. Ask for a second opinion and the doctor's rationale if he or she suggests this process. Magnetic resonance imaging's use is limited by cost and patient intolerance, as the process can be time-consuming and uncomfortable. Low signal intensity on T1-weighted images suggests iron overload from hereditary hemochromatosis.
Get a biopsy for a definitive diagnosis. Checking for signs and symptoms and running blood tests are all good methods for confirming a suspicion of cirrhosis. However, the only way to know for certain that a liver is cirrhotic is to allow a doctor to perform a biopsy on it. After processing and examining the liver sample under a microscope, the doctor will be able to say for sure whether the patient has cirrhosis.
Receiving Treatment for Cirrhosis
Allow medical staff to direct your treatment. For cases of cirrhosis, most mild to moderate cases are handled on an outpatient basis, with some exceptions. If the patient has major gastrointestinal bleeding, severe infection or sepsis, kidney failure, or altered mental status, treatment in the hospital is required. The doctor will likely ask you to abstain from alcohol, drugs, and medications if you have liver toxicity. The doctor will evaluate this on an individual basis. Additionally, certain herbs like kava and mistletoe can cause further damage to your liver. Discuss all herbal/alternative treatments you are currently taking with your doctor. Your doctor will immunize you against pneumococcal disease, influenza, and hepatitis A and hepatitis B. Your doctor will also establish the NASH protocol for you, in which you will be put on a plan for weight reduction, exercise, and optimal control of lipids and glucose (fats and sugars/carbohydrates).
Take medications as directed. As discussed in previous sections, many underlying causes lead to cirrhosis. The medication your doctor prescribes will be very customized and specific to your precise case. These drugs will treat underlying causes (Hepatitis B, Hepatitis C, biliary cirrhosis, etc.) as well as the symptoms that result from cirrhosis and subsequent liver failure.
Be prepared for surgical options. Doctors don't always suggest surgery, but may recommend it if certain conditions arise from the cirrhosis. These conditions include: Varices, or dilated blood vessels and can be treated with ligation (surgically tying off the vessel). Ascites, an abdominal fluid buildup that's treated with paracentesis, a draining procedure. Fulminant hepatic failure, a rapid onset of encephalopathy (alteration of brain structure/function within 8 weeks of diagnosed liver cirrhosis). This condition calls for a liver transplant. Hepatocellular carcinoma is the development of liver cancer. Attempts at treatment include radiofrequency ablation, resection (surgical removal of the carcinoma), and liver transplant.
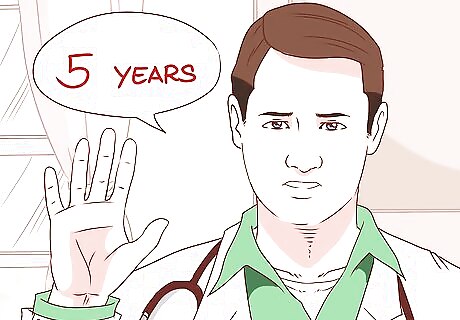
Understand your prognosis. After a diagnosis of cirrhosis, people can usually expect 5-20 years of life with the disease with little or no symptoms. Once severe symptoms and complications arise from cirrhosis, death within 5 years without transplant is common. Hepatorenal syndrome is one severe complication that may occur due to cirrhosis. This refers to the development of renal failure in patients with liver disease, requiring treatment for kidney failure. Hepatopulmonary syndrome, another serious complication, is caused by the broadening of the arteries in the lungs of patients with liver disease. It leads to shortness of breath and hypoxemia (low oxygen levels in the blood). The treatment for this is a liver transplant.

















Comments
0 comment