views
- Roll, stretch, or stimulate the nipple with your fingers to encourage protrusion.
- Consider devices like breast shells or pumps or a Niplette to draw the nipple out, especially if you’re preparing to breastfeed.
- Inverted nipples might be a sign of an underlying condition if they've changed since you turned 50. Ask a doctor about concerns or corrective surgery.
Making a Plan
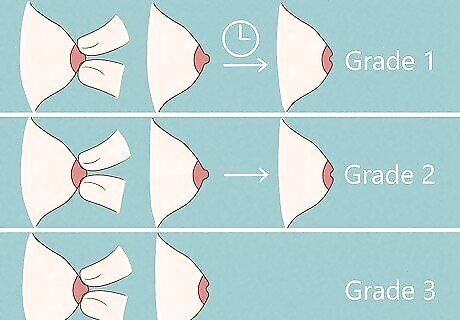
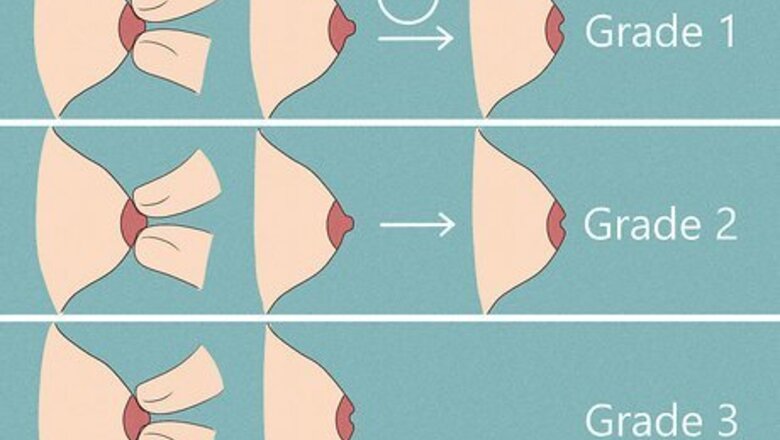
Determine the grade of your inverted nipples. Take off your shirt and stand in front of a mirror. Holding your breast at the edge of the areola (the dark area of skin surrounding the nipple) between your thumb and forefinger, press inwards about an inch behind your nipple. Be firm but gentle. Depending on the nipple's response, you can assess the grade of inversion. Grade 1: The nipple protracts easily when you apply light pressure to the areola. When pressure is released, the nipple maintains its projection, rather than retracting immediately. Grade 1 inverted nipples are unlikely to interfere with breastfeeding, though you still may have cosmetic concerns. There is little to no fibrosis (excess connective tissue) in Grade 1 inverted nipples. Grade 2: The nipple protracts when pressure is applied, though not very easily, and retracts as soon as pressure is released. Grade 2 inversions are more likely to complicate breastfeeding. There is often a moderate degree of fibrosis, with mild retraction of the lactiferous or milk ducts. Grade 3: The nipple is retracted and does not respond to manipulation; it cannot be pulled out. This is the most serious form of inversion, with a significant amount of fibrosis and retracted milk ducts. You may also experience rashes or infections if you have Grade 3 inversion, and breastfeeding may be impossible. Test both nipples, since they may not both be inverted.
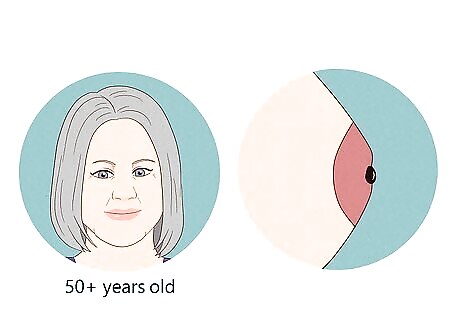
Identify the cause. If you have had inverted nipples since childhood or puberty, your nipples are unlikely to indicate an underlying problem. If they have changed recently, especially if you are over 50, they could indicate an illness or infection. Cancer and other serious conditions like inflammation or infection can occasionally cause inverted nipples. If you are over 50 and your areola appears distorted and your nipple appears flatter than normal, or has become inverted, get screened for breast cancer immediately. Women and some trans people over 50 are at risk for developing Paget's disease of the breast. Pink discharge and crusting, thickening, flaking, or scaling of the skin of the nipple and areola can also be symptoms of breast cancer. See a doctor if you have dirty white, greenish, or black discharge from your nipple. Tenderness, redness, or a breast lump may be a sign of mammary duct ectasia. Perimenopausal people are especially at risk for mammary duct ectasia. If you develop a painful lump that oozes pus when pushed or cut, and if you have a fever, you may have a type of infection called subareolar breast abscess. Most nipple infections happen during lactation, but subareolar breast abscesses appear in people who are not lactating. If your nipples have been recently pierced and you’re experiencing symptoms of a breast abscess, consult your doctor.
Decide on a treatment method. The treatment method depends on the grade of your inversion, the cause of your inversion, and whether you are planning to breastfeed. If you have signs of breast cancer, infection, or mammary duct ectasia, visit your doctor immediately. If you have Grade 1 inversion, it's likely that manual methods can help loosen the fibrous tissue and allow the nipple to protract more easily. If you have Grade 2 or 3 inversion, it may be a good idea to consult a doctor for your treatment plan. In some cases, non-invasive methods may be adequate, while plastic surgery may be a better option in others. If you are pregnant or nursing, be guided by your doctor, nurse or lactation consultant.
Manual Training
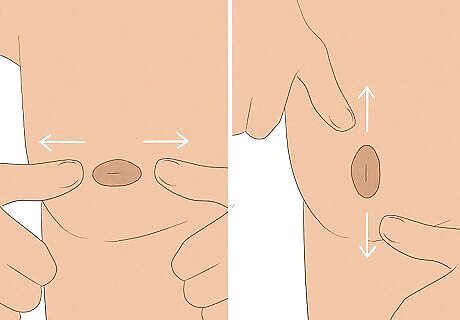
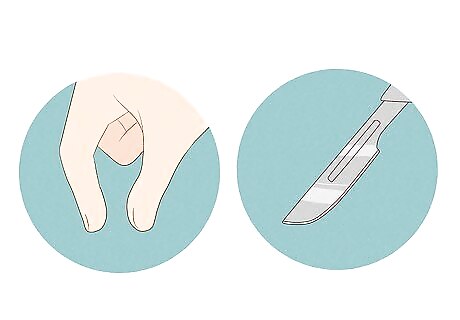
Use the Hoffman technique. Place both thumbs on opposite sides of the nipple at the base. Gently pull the thumbs away from each other in opposite directions. Work both up and down and sideways. Try doing multiple repetitions with your fingers in a horizontal and vertical position. This technique is thought to break down the adhesions at the base of the nipple that keep it inverted.
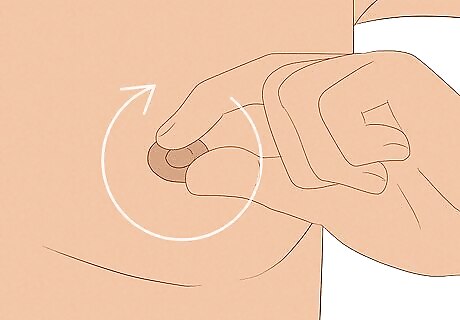
Roll your nipple between thumb and forefinger several times a day. Pull on the nipple gently when it is erect to encourage it to stay so. Afterward, wet a towel with cold water and apply it to your nipples to stimulate them further.
Using Products
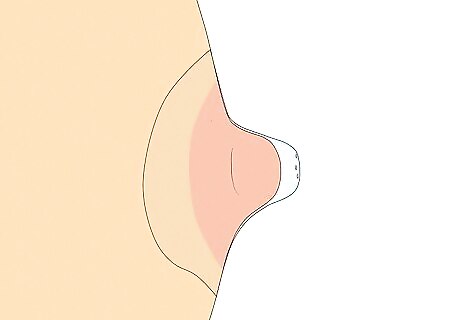
Use breast shells. Breast shells are sold at maternity stores and online. They are soft, circular discs with a small hole in the middle that pushes the nipple forward. Cup your breast inside the shield and position your nipple through the small hole. Wear the breast shell under your shirt, undershirt, or bra. You may need to have an extra layer of clothing to hide it adequately. If you are preparing to nurse, wear the shell for 30 minutes prior to breastfeeding. The shell applies gentle pressure to your nipple to encourage it to stay erect. It can be used by anyone as a treatment for inverted nipples. The breast shell may stimulate lactation in people who breastfeed. Nursing parents should not wear them continuously for days on end. If you wear the shell during feedings, be sure to wash it in hot, soapy water afterward, and dispose of any milk leaked into the shell during wearing. Monitor the area around your breast when using breast shells, as they may cause rashes.
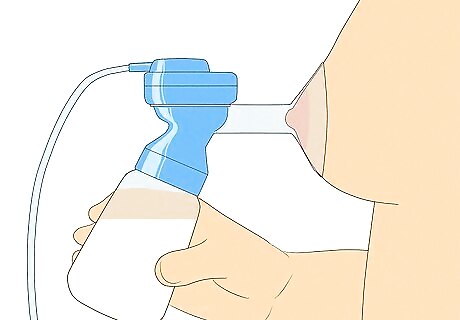
Use a breast pump. If you are pregnant or nursing, use your breast pump to evert the nipple tissue. Place the phalange over your breast, ensuring your nipple is centered inside the hole. Phalanges come in different sizes, so be sure the phalange you're using covers your nipple. Hold the phalange against your breast, ensuring a seal against your skin. Holding the phalange or bottle in one hand, turn on the pump. Pump at the highest comfortable strength. Use a low speed when you’re starting out. Turn off the machine by holding both bottles against you with one arm and turning off the pump with another. If you are nursing, give the nipple to your baby once your nipple is erect. Don’t pump extensively if you are nursing, since it will start the flow of milk from your nipple. There are a variety of breast pumps on the market; high-quality electric pumps like those used at a maternity ward do the best job of pulling the nipple out without damaging surrounding tissue. Breast pumps vary from one manufacturer to another. Talk to a nurse or lactation consultant about the best way to use the particular pump you're working with.
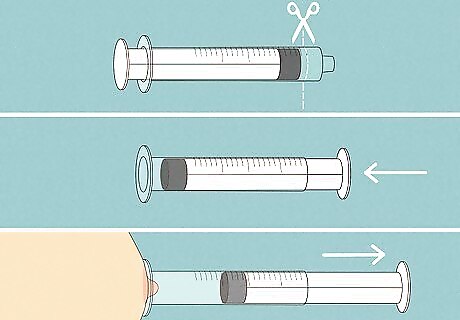
Use an inverted syringe. Pull out your nipple using a clean, needleless 10 milliliters (0.34 fl oz) syringe (this size may vary depending on your nipple size). Use clean, sharp scissors to cut off the end of the syringe where it reads "0 mL". (The side opposite to the plunger.) Remove the plunger and reinsert it at the end you just cut off, pushing the plunger all the way in. Place the uncut end over your nipple and draw out the plunger so that your nipple protracts. Do not pull farther than is comfortable. Before removing, push the plunger slightly back in to break the suction. Once finished, disassemble all parts and wash with hot, soapy water. If you prefer, there is a medical device called Evert-It, which is a modified syringe with a breast phalange. It works on the same principle described above.
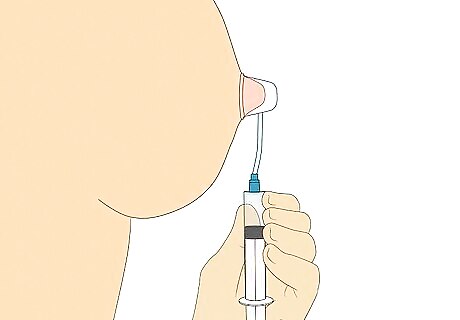
Use the Niplette. The Niplette is a device that elongates the milk ducts by pulling on the nipple for an extended period. This small, clear, plastic device is worn over the nipple and under clothing. Apply a small amount of nipple ointment to the nipple and areola and the base of the Niplette. Insert the syringe into the open end of the valve, pushing firmly. Place the Avent Niplette over your nipple with one hand and pull the syringe with the other, creating suction. Don't pull too hard - this should not be painful! Once the nipple has been pulled out, release the Niplette. Grasp the valve and carefully remove the syringe from the valve. Do this carefully so that no air is re-injected, which would cause the device to fall off. Wear your Niplette under your clothing. If you're wearing a tight top, you can conceal the Niplette with a specially designed protective cover. Remove the Niplette by pushing the syringe into the valve to break the vacuum. Start by wearing the Niplette for one hour per day. Gradually increase by one hour each day, working up to eight hours per day. Do not wear the Niplette day and night! Within three weeks you should see results, with the nipple filling the mould.
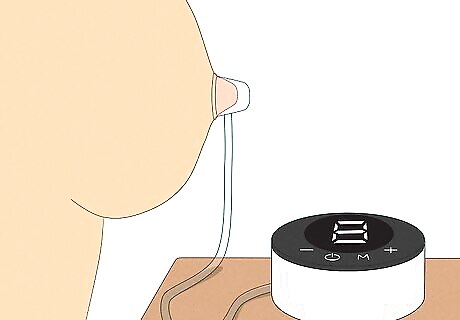
Use the Electric Nipple Corrector. There are 4 modes and 9 levels of suction for this electric nipple corrector, which can be selected according to individual needs. And the soft material of suction cups will not make your nipples suffer. The suction cups do not easily fall off during use. Connect the suction cups and the tube together. Install the tube connected with the suction cups to the machine. Put the suction cup on the nipples, long press the power button to start the machine, short press the power button to select modes, press "+" or "-" to adjust gears, and then start to correct. The electric nipple corrector is suitable for inverted nipples for grades 1 and 2. It is recommended to use 1-2 times a day, 15-20 minutes each time, and the interval between two corrections should be about 5-8 hours. Generally, nipples will evert after 7-10 days of continuous use. After 3 months of continuous use, the inverted nipples are basically corrected, and not easy to get inverted again. If you prefer, there is a device called Rolevin Nipple Corrector. It works on the same principle described above.
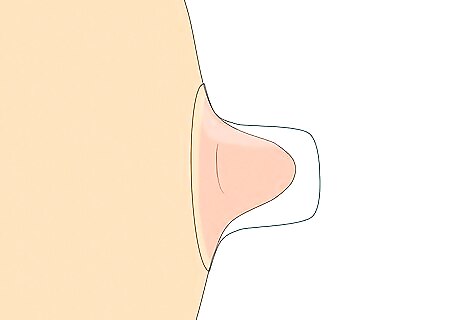
Use Supple Cups. Supple Cups sold online have been designed to help address flat, shy and inverted nipples, by drawing the nipple into the cup. A very small study showed they may help. Center the Supple Cup onto the nipple and squeeze the bottom of the Supple Cup as you gently press it onto the nipple. This creates a gentle vacuum, drawing the nipple into the Supple Cup. For an improved seal, apply a small amount of nipple cream or butter – such as USP modified lanolin – on nipple and interior of the Supple Cup. If that still doesn’t work, you may want to try a different size. New users typically wear Supple Cups for 15 minutes on the first day. If no pain or discomfort is experienced, one may advance the time each day, gradually increasing to four hours per day by the end of the first week. Some are able to wear the Supple Cups under a bra without the Supple Cup being displaced or without discomfort. Alternatively, Breast Shells can be used in conjunction with Supple Cups to prevent a tight bra from flattening out the Supple Cups, causing uncomfortable pressure, or being detached from the nipple.
Medical Treatment
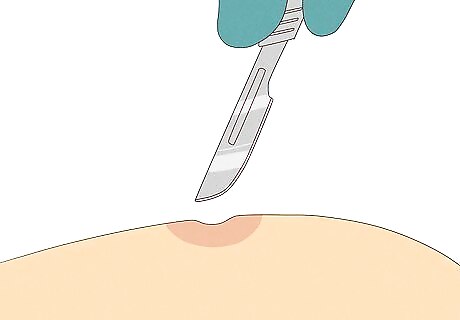
Talk to your doctor or plastic surgeon about corrective surgery. While it may be desirable to correct the issue non-surgically, for some people surgery is a good option. Newer methods can do so without severing the milk ducts, making it possible to breastfeed after the procedure. Your doctor or plastic surgeon can help you decide whether you are a good candidate for corrective surgery. This is a short outpatient procedure involving local anesthesia. You can go home the same day, and, because it is minimally invasive, you will probably be able to return to your routine (work, etc.) the following day. Discuss the procedure with your surgeon. Inform yourself about how the procedure is performed, and what results you can expect. At this time your surgeon will examine your medical history and assess the underlying cause of your condition.
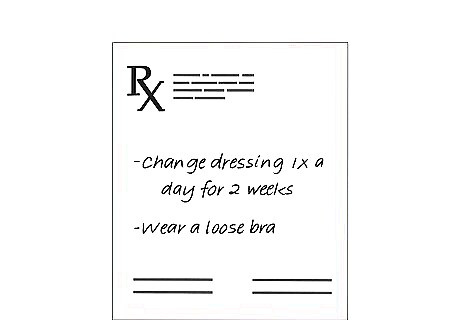
Follow pre-operative and post-operative instructions carefully. Your surgeon will inform you about how to prepare for surgery and what to do afterwards. You will likely have surgical dressings on your nipple after the operation. Change these dressings if and as instructed by your surgeon.

After the operation, report any questions or concerns to your surgeon. Recovery should be relatively painless. If you experience unexpected bruising, swelling, or discomfort during recovery, contact your surgeon immediately.

Schedule a post-operative visit with your surgeon. These visits assess the progress of your healing and the success of the procedure. Ask your surgeon when you should come in for your follow-up.
















Comments
0 comment