
views
X
Research source
In order to diagnose POTS, you will need to see your doctor. They can then evaluate your vital signs with postural changes, and also assess for the presence of other symptoms that may be present with a POTS diagnosis.
- Look out for symptoms of POTS including fatigue, lightheadedness or fainting, heart palpitations, or shaking when you stand up.
- Visit a doctor for a diagnosis if you’re experiencing symptoms. Inform them of all medications you take, and have them take your heart rate and blood pressure.
- Get a “tilt table test” for a thorough diagnosis. A doctor will monitor your vitals as you lay on a table that gradually tilts from horizontal to vertical.
Recognizing Symptoms
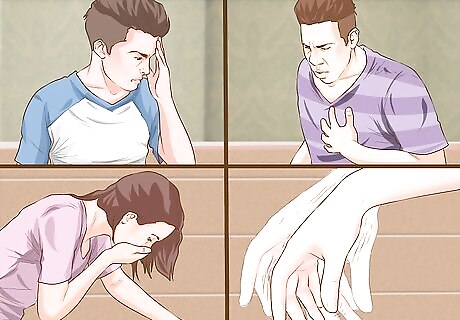
Recognize signs and symptoms that may accompany a POTS diagnosis. In addition to an elevated heart rate upon standing, people with POTS may experience a variety of others symptoms. These include: Unusual fatigue Headaches Lightheadedness and/or fainting Exercise intolerance, with or without chest pain and shortness of breath Heart palpitations (meaning episodes of unusual heart rhythms) Nausea and/or vomiting Diminished concentration Shaking and/or tremors Problems with the nerves (the nervous system) that affect other areas of the body
Notice if you have had any recent triggers that may cause POTS. Oftentimes an infection (such as mononucleosis) can be a trigger for POTS. Other common triggers include pregnancy and stress. With that said, POTS may also occur without an observable trigger. A number of studies have associated POTS with cardiovascular deconditioning.

Be aware of who is at greater risk. People who are at an increased risk of developing POTS include women, people between the ages 12 and 50, and those who have been exposed to triggers (such as an infection, pregnancy, and/or stress). People taking multiple medications may also be at increased risk of noticing symptoms. This is because certain blood pressure medications and heart-related medications may exacerbate the signs and symptoms of POTS.
Visiting a Doctor
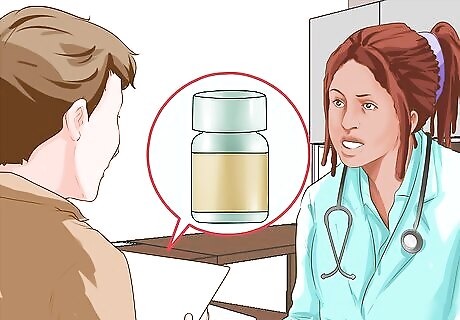
Bring a list of your current medications to your doctor. As you prepare for your visit with your physician, it is important to have a list of all your current medications on hand, including the names of the medications, the doses, and the reason you are taking each one. It is also important to have a list of your past medical history, including any surgeries or hospitalizations from your past, as well as any ongoing health concerns that you have suffered from. This information will help your doctor to understand your whole health history better, so that he can evaluate your risk of POTS and move forward with diagnostic testing.

Have your doctor measure your heart rate sitting and standing. POTS is a form of "autonomic dysregulation" (a nervous system disorder) in which your heart rate spikes upon standing (among other symptoms). In order to diagnose POTS, your doctor will need to measure your heart rate when you are sitting at rest. You will then stand and, after one or two minutes, your doctor will measure your heart rate again. If your heart rate increases by 30 BPM (beats per minute) or more when you stand, this means that you have POTS.
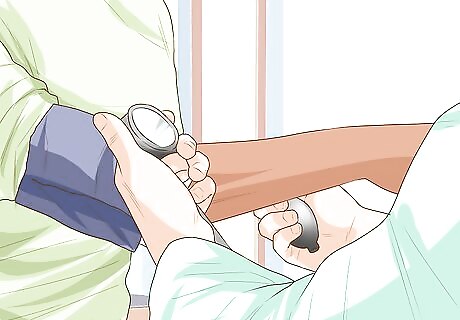
Have your blood pressure measured as well. After your doctor measures your heart rate and its variance when you are sitting versus standing, she will also want to measure your blood pressure. The reason for this is to rule out a condition called "orthostatic hypotension" (this is when your blood pressure drops significantly when you stand, leading to a compensatory elevated heart rate). Because your doctor does not want to diagnose you with POTS if you actually have orthostatic hypotension (that is, if your blood pressure is actually more of a problem than your heart rate), she will need to measure your blood pressure while sitting, then again after you stand up. If you have POTS and not orthostatic hypotension, then your blood pressure should not drop significantly when you stand up versus when you are sitting. Alternatively, if your resting heart rate is above 120 BPM when you stand, this is also in itself diagnostic of POTS.

Know that the heart rate criteria are different for children and adolescents. Children and adolescents have naturally faster heart rates than adults; therefore, their heart rate must increase by at least 40 BPM (beats per minute) when they make the transition from sitting to standing, in order to be diagnosed with POTS.

Receive a "tilt table test." Your doctor can diagnose you with POTS by simply measuring your heart rate sitting and standing; alternatively, he or she may perform what is called the "tilt table test." This is a much lengthier and more detailed exam. In total, it takes between 30-40 minutes to do the simple version, and up to 90 minutes to do the complex version. The tilt table test is where you lie on a table that changes positions at set time intervals. As this occurs, you are attached to machines such as an ECG and blood pressure cuff to continuously monitor your vital signs, including heart rate and rhythm, and blood pressure. Your doctor can evaluate the series of results and use this to diagnose POTS or other heart-related conditions.
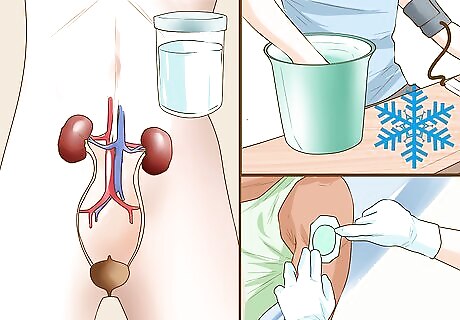
Talk to your doctor about other tests. There are many other tests that can be used to aid in the diagnosis of POTS. Your doctor may suggest a catecholamine test, a cold pressor test, EMG (electromyographic) testing, and sweat tests, among other things. POTS is a heterogeneous disorder, meaning that it can manifest in a variety of ways and have different underlying causes. As a result, the best set of diagnostic tests to confirm the details of your POTS diagnosis will depend upon your doctor's assessment of your particular case.

Be aware of the implications that POTS can have on your quality of life. Approximately 25% of people diagnosed with POTS have impaired quality of life similar to someone who is officially categorized as disabled. This includes not being able to work, as well as possible difficulty with day-to-day tasks such as bathing, eating, walking, or standing; however, while some people with POTS suffer from a reduced quality of life, others are able to live normally and you might not know they have a medical condition unless they told you. The prognosis for POTS is highly variable from case to case. For POTS where the onset follows a viral infection (termed a "post-viral episode"), approximately 50% of patients recover in two to five years time. If you have been diagnosed with POTS, your doctor can provide you with information that is specific to you in terms of prognosis, as well as working with you to develop a personalized treatment plan. Your prognosis will depend upon the subtype of POTS that you have, your overall health history, the underlying cause of your disorder, and the constellation of symptoms (as well as the symptom severity) that you are experiencing. Non-pharmacological measures for the treatment of POTS include eliminating aggravating factors, addressing dehydration, and increasing activity. As far as medication goes, there have been no-long term studies on the efficacy of medications to treat POTS and all medication is used off label.

















Comments
0 comment